Journal of Gastroenterology Research and Practic
Case Report - Open Access, Volume 3
Ectopic duodenal mucosa with adenomatous hyperplasia in the stomach: A case report
Xiaowei Cai; Lin Li; Yanxia Yang; Kang Lu; Peng Wang*
The 985th Hospital of the Joint Logistics Support Force, Qiaodong Road No.30, Taiyuan 030001, China.
*Corresponding Author : Peng Wang
Department of Pathology, the 985th Hospital of the
Joint Logistics Support Force, Qiaodong Road No.30,
Taiyuan 030001, China.
Tel: +86-15235397070; Email: lukang11100@163.com
Received : May 01, 2023
Accepted : Jun 05, 2023
Published : Jun 15, 2023
Archived : www.jjgastro.com
Copyright : © Wang P (2023).
Abstract
A 49-year-old man presented with abdominal distension and loss of appetite for 1 month as the main symptoms. Gastroscopy revealed a space occupying lesion in the pylorus of gastric antrum. After electroresection, pathological and immunohistochemical examination showed that it was “ectopic duodenal mucosa with adenomatous hyperplasia in the stomach”. This disease has not been reported so far. After short-term follow-up and endoscopic review of this patient, we concluded that this disease is an extremely rare gastric tumor with benign growth and good prognosis after endoscopic resection with high-frequency electrocautery. This case helps us to recognize the pathology and treatment of this disease, which is helpful for the differential diagnosis of other gastric space-occupying diseases
Keywords: Ectopic duodenal mucosa; Adenomatous hyperplasia; Stomach; Tumor.
Citation: Cai X, Li L, Yang Y, Lu K, Wang P. Ectopic duodenal mucosa with adenomatous hyperplasia in the stomach: A case report. J Gastroenterol Res Pract. 2023; 3(4): 1144.
Introduction
Gastric neoplasm is a very common digestive disease, and different types of tumors are treated differently [1]. Ectopic duodenal mucosa with adenomatous hyperplasia in the stomach has not been reported previously. We encountered a case of intragastric tumor in September 2022, which was confirmed by pathology as ectopic duodenal mucosa with adenomatous hyperplasia in the stomach. According to our experience, a case of diagnosis and treatment of this disease reported with the literature review.
Case presentation
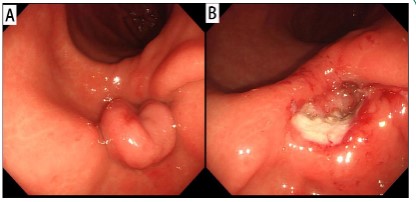
A 49-year-old man presented with a complaint of abdominal distension with decreased appetite for one month. The patient had no abdominal pain, hematemesis, melena, or other symptoms. There was no history of weight loss or family history of gastrointestinal disease. Other vital signs were normal. Abdominal physical examination showed no obvious abnormalities. Laboratory tests showed normal blood routine and tumor markers. Fecal occult blood was negative. Gastroscopy revealed a mucosal protuberous lesion in the greater curvature of the stomach, about 2.0 cm × 3.0 cm in size, extending to the pyloric canal, which was resected by high-frequency electric coil (Figure 1). The pathological diagnosis was ectopic gastroduodenal mucosa with adenomatous hyperplasia.
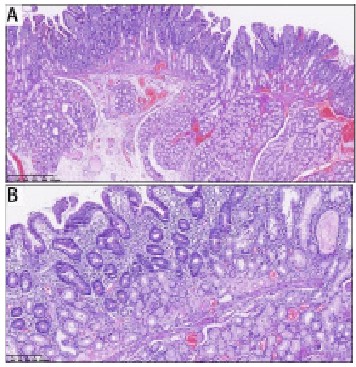
Pathological structure under microscope
The surface of the tumor was the duodenal mucosa, with columnar brush border cells, scattered goblet cells, Panes cells and the intrinsic glands of the duodenal mucosa. There were focal infiltration of lymphocytes and scattered eosinophils in the stroma of the lamina propria, accompanied by hyperemia and edema, and telangiectasis. The duodenal glands showed adenomatous hyperplasia at the base of the lamina propria and the submucosa, which were surrounded by mucosal smooth muscle fibers and divided into lobules. The glandular epithelium was well differentiated without atypia. At the base of the tumor, there were proliferating collagen fibrous connective tissue (Figure 2).
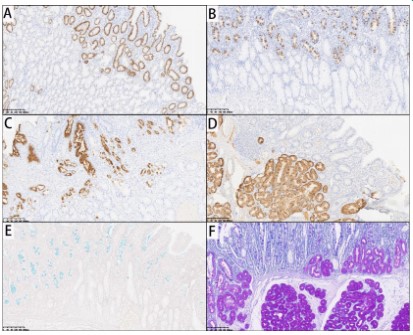
The specific gastric and intestinal epithelial immunohistochemical markers were further examined, such as MUC2, CD-X2, villin and AB-PAS staining. The results suggested that the tumor originated from the mucosa of the duodenum, rather than intestinal metaplasia of the gastric mucosa (Figure 3).
Therapy and follow up
We performed endoscopic high-frequency electric snare resection for this patient. The obstruction symptoms were significantly relieved after surgery. Half a year later, gastroscopy reexamination showed that the wound and ulcer of gastric antrum mucosa healed well. After half a year of follow-up, the patient had no discomfort symptoms and no recurrence.
Discussion
Ectopic duodenal mucosa with adenomatous hyperplasia in the stomach is extremely rare in clinical practice. In this paper, we describe a protuberant lesion in the gastric antrum, finally was pathologically diagnosed as ectopic duodenal mucosa. We hold the opinion that this disease is an adenomatoid hyperplasia of the duodenal gland on the basis of duodenal mucosa ectopia in stomach. Pathological examination showed that the tissues were well differentiated, with no obvious atypia and a benign development process.
Clinical analogues of this disease are gastric adenomas, pyloric adenomas, and gastric polyps. Duodenal Brunner adenoma is similar with this disease.
Gastric adenomas are benign polypoid lesions composed of neoplastic gastric epithelium, accounting for about 10% of gastric benign polypoid lesions, also known as adenomatous polyps or gastric polypoid dysplasia. Its nature belongs to gastric mucosal dysplasia/intraepithelial neoplasia, which is the precursor lesion of gastric cancer. They were divided into intestinal adenoma, pyloric adenoma, foveolar adenoma and acid-secreting adenoma [2].
Pyloric gland adenoma (Pyloric gland adenoma) is a rare gastrointestinal tumor. Gastric pyloric adenomas arise in chronically damaged mucosa. The neoplastic glands had the differentiation of gastric pyloric glands and were tightly organized with occasional cystic dilatation. Individual cells were cuboidal to columnar, with eosinophilic to amphoteric cytoplasm, and imucosal or mucinous tectum poorly formed. The nuclei were round to ovoid with occasional prominent nucleoli. By immunohistochemistry, tumor cells marked gastric pyloric gland differentiation markers, including MUC6 and MUC5AC [3]. Although its pyloric adenoma can be treated conservatively, it should be completely removed if possible, especially for large adenomas or pyloric adenomas showing high-grade features [4].
Gastric polyps are sessile or pedunculated lesions that originate from the gastric epithelium or submucosa and protrude into the gastric cavity. Malignant potential: According to the histological type, some gastric polyps (adenomas and hyperplastic polyps) have malignant potential and are a precursor to early gastric cancer. They may also indicate an increased risk of intestinal or extraintestinal malignancies [5].
Duodenal Brunner adenoma refers to the presence of fundic gland tissue in the lamina propria mucosa of the duodenal bulb, that is, well differentiated gastric glands containing com- plete chief cells and parietal cells can be seen in the lamina propria mucosa of the duodenal bulb. They were usually polypoid nodules, granular or flat uplift, part of the gastric mucosa wrinkle-like uplift, cobblestone-like uplift, cauliflower-like uplift, etc., with different sizes and numbers, often multiple. Duodenal Brunner adenoma should be removed early and examined pathologically to prevent serious complications [6].
Conclusion
In summary, ectopic duodenal mucosa with adenomatous hyperplasia in the stomach is generally benign. In order to confirm the diagnosis and avoid canceration, ulcer, bleeding and other complications, complete endoscopic resection of the goitre with pathological examination is appropriate.
References
- Tham E, Sestito M, Markovich B, Garland-Kledzik M. Current and future imaging modalities in gastric cancer. J Surg Oncol. 2022; 125: 1123-1134.
- Kushima R, Vieth M, Borchard F, Stolte M, Mukaisho K, et al. Gastric-type well-differentiated adenocarcinoma and pyloric gland adenoma of the stomach. Gastric Cancer. 2006; 9: 177-184.
- Pezhouh MK, Park JY. Gastric pyloric gland adenoma. Arch Pathol Lab Med. 2015; 139: 823-826.
- Choi WT, Brown I, Ushiku T, Yozu M, Setia N, et al. Gastric pyloric gland adenoma: a multicentre clinicopathological study of 67 cases. Histopathology. 2018; 72: 1007-1014.
- Goddard AF, Badreldin R, Pritchard DM, Walker MM, Warren B. The management of gastric polyps. Gut. 2010; 59: 1270-1276.
- Lu L, Li R, Zhang G, Zhao Z, Fu W, et al. Brunner's gland adenoma of duodenum: report of two cases. Int J Clin Exp Pathol. 2015; 8: 7565-7569.