Journal of Gastroenterology Research and Practice
Research Article- Open Access, Volume 3
Endoscopic fluoroscopy: A technique to diagnose disorders of intestinal rotation
Alyssa R Mowrer1*; Christina M Bence1; Alfonso M Martinez2; Amy J Wagner1
1Division of Pediatric Surgery, Department of Surgery, Medical College of Wisconsin, Milwaukee, Wisconsin, USA.
2Division of Pediatric Gastroenterology, Medical College of Wisconsin, Milwaukee, Wisconsin, USA.
*Corresponding Author : Alyssa R Mowrer
Division of Pediatric Surgery, Department of Surgery,
Medical College of Wisconsin, Milwaukee, Wisconsin,
USA.
Tel: 1-414-266-6558; Email: amowrer@chw.org
Received : Mar 27, 2023
Accepted : Apr 24, 2023
Published : Apr 28, 2023
Archived : www.jjgastro.com
Copyright : © Mowrer AR (2023).
Abstract
Background: Intestinal malrotation with Ladd’s bands is the most common cause of congenital extrinsic duodenal obstruction and the gold-standard for diagnosis is Upper Gastrointestinal series (UGI). However, a subset of patients presents with symptoms of chronic partial duodenal obstruction despite normal UGI. A novel technique, termed Endoscopic Fluoroscopy (EF), for the diagnosis of Occult Intestinal Rotational Abnormalities (OIRA) may assist this patient population in obtaining an accurate diagnosis and subsequent treatment plan.
Methods: EF involves a combination of esophagoduodenoscopy and duodenal fluoroscopy, allowing for improved visualization of anatomy, intestinal caliber, and motility when compared to traditional UGI. A retrospective review of patients <18 years of age who underwent a Ladd Procedure following diagnosis of OIRA on EF was performed at a tertiary care children’s hospital from 2012-2019.
Results: The most common presenting symptoms for the study population were feeding intolerance (79%), emesis (64%), and failure to thrive (43%). Age at operation ranged from 3 months to 13 years. Findings on EF concerning for OIRA included duodenal tortuosity, or hairpin turns with an associated intestinal caliber change. Postoperatively, 64% of patients had complete symptom resolution by 60-days after the procedure and all patients demonstrated improved trajectories on the growth curve.
Conclusions: EF is a novel technique for diagnosing OIRA due to Ladd’s bands not identified on traditional imaging studies. Preliminary experiences at this institution with EF demonstrate its effectiveness as a diagnostic modality to identify patients that would likely benefit significantly from a Ladd procedure.
Keywords: Esophagoduodenoscopy; Malrotation; Intestine; Ladd’s bands.
Citation: Mowrer AR, Bence CM, Martinez AM, Wagner AJ. Endoscopic fluoroscopy: A technique to diagnose disorders of intestinal rotation. J Gastroenterol Res Pract. 2023; 3(3): 1138.
Introduction
Intestinal malrotation is the most common cause of congenital extrinsic duodenal obstruction. Malrotation is a broad term that encompasses a spectrum of abnormal intestinal rotational states resulting from errors in normal embryologic bowel development [1]. It is associated with fibrous peritoneal adhesions called Ladd’s bands that stretch across the duodenum and can result in extrinsic obstruction [2]. Clinically, malrotation can range from an asymptomatic finding on imaging, to life-threatening bowel ischemia due to midgut volvulus [3]. The current gold standard for diagnosing malrotation is an upper gastrointestinal series (UGI) contrast study demonstrating malposition of the duodenojejunal junction [1]. While the sensitivity of UGI for diagnosing classic malrotation is cited as high as 96%, there remains a subset of patients that manifest symptoms of chronic intestinal obstruction yet demonstrate equivocal or negative findings on UGI [4].
A review of the literature identifies a number of case reports and small series that describe patients with chronic gastrointestinal symptoms persisting into childhood and even adulthood that are ultimately determined to be due to subtle rotational abnormalities of the intestine with symptomatic Ladd’s bands [5-9]. The mainstay of treatment for malrotation is the Ladd procedure, which involves laparoscopic or open lysis of Ladd’s bands, widening of the mesentery, derotation of the intestines, placing the small bowel on the right side and colon on the left side of the abdomen, and incidental appendectomy. The difficulty lies in identifying the patients that have symptomatic subtle rotational abnormalities with equivocal or negative findings on UGI who would ultimately benefit from a Ladd procedure.
Currently, there is no “gold standard” for diagnosing patients with subtle intestinal rotation abnormalities who have negative or equivocal findings on UGI [1]. Some patients require diagnostic laparoscopy or laparotomy if clinical suspicion is high, which involves the risk of a negative or unnecessary operation [9]. There is a clinical need for a less invasive diagnostic technique that can more accurately identify patients with occult rotational abnormalities who would benefit from a Ladd procedure. The purpose of this study was to review outcomes associated with Endoscopic Fluoroscopy (EF), a technique for diagnosing occult intestinal rotational abnormalities that is being utilized as a collaborative effort between our Pediatric Surgery and Pediatric Gastroenterology teams.
Materials and methods
Endoscopic fluoroscopy
EF is a technique that involves direct visualization of the duodenum via upper endoscopy, followed by injection of water-soluble contrast through the endoscope to allow for dynamic fluoroscopic examination of the duodenum in real-time. The contrast protocol utilizes Omnipaque 240 mOsm diluted and dosed in volumes ranging from 30-90 ml depending on patient size. EF is currently being employed by a single gastroenterologist at our children’s hospital for patients that present with symptoms of chronic duodenal obstruction (e.g., intolerance of oral feeds, failure to thrive) who have had an otherwise non-diagnostic workup, including UGI. The next step in the workup for chronic upper gastrointestinal symptomatology in a pediatric patient is commonly upper endoscopy. EF is performed as an adjunct with the upper endoscopy procedure in this specific population of patients and therefore does not require a separate anesthetic or additional procedure. If the findings on EF are concerning for abnormal rotation or obstructing Ladd’s bands, the patient is referred to the Pediatric Surgery service for consideration of a Ladd procedure.
Study design
To evaluate the efficacy of EF in patient selection for operative intervention due to occult intestinal rotational abnormalities, a retrospective review of patient outcomes at a single tertiary care children’s hospital was performed following Institutional Review Board approval. All patients <18 years of age who underwent a Ladd procedure following diagnosis of occult intestinal rotational abnormality by EF between January 2012 and January 2019 were included in the study. Exclusion criteria were other causes of intestinal obstruction (annular pancreas, SMA syndrome, intestinal atresia/stenosis, or post-surgical adhesions) and primary operation at an outside institution. Patients were identified using diagnostic and procedure codes and eligibility was confirmed via review of the medical record.
Data collection
Demographic data were collected that included patient age, gender, race, gestational age, birth weight, and medical comorbidities. Findings on preoperative workup were evaluated, including type and duration of symptoms, weight-for-age trends, findings on UGI, and prior therapies or procedures. Feeding intolerance was classified as any volume-limiting post-prandial abdominal pain, emesis, or gastrostomy tube leakage/venting. Failure to thrive was defined as two or more consecutive weights below the 5th percentile for age documented in a patient’s electronic growth chart, or documentation by a provider of failure to thrive during preoperative workup. Medically refractory reflux was defined as an active diagnosis of reflux despite the patient currently taking at least one anti-reflux medication. Perioperative characteristics collected included findings documented on EF, operative procedures performed, and intra-operative surgical observations. Postoperative variables of interest were complications, hospital length of stay, and presentation at 60-day follow-up including weight trends, persistent gastrointestinal symptoms, and tolerance of oral feeds.
Statistical analysis
Patient characteristics and outcomes were described through summary statistics, using medians with ranges for continuous variables and frequencies with percentages for categorical variables. To analyze comparative data, McNemar’s test was used for paired binary variables and student’s t-test was used for paired continuous variables. A p-value of <0.05 was considered statistically significant.
Results
Demographics and preoperative characteristics
A total of 14 patients underwent a Ladd procedure following a diagnosis of occult intestinal rotational abnormality on EF during the study period, and patient characteristics are described in Table 1. Seventy-one percent of the study population were male with a median age at diagnosis of 6.3 months (range = 3 months-13 years). Eight patients (57%) were white/Caucasian, three (22%) were black/African American, and one of each of the remaining three patients (7%) were Hispanic/Latino, American Indian, and unknown race. The median gestational age at birth was 39.5 weeks (range = 24-41 weeks) with 21% of patients born at <37 weeks gestation. Similarly, 21% of patients had a birth weight of <2.5 kg and median birth weight was 3.0 kg (range = 0.7-3.6 kg). Five patients (36%) had other medical comorbidities including asthma (2/14), diabetes (1/14), and tracheal stenosis (1/14). One patient born at 24 weeks gestation had a prolonged neonatal intensive care unit stay that was complicated by necrotizing enterocolitis requiring peritoneal drainage and developed oral aversion requiring gastrostomy tube placement prior to diagnosis of abnormal intestinal rotation. No other patients had undergone surgical procedures prior to EF.
Median duration of GI symptoms prior to diagnosis was 5.5 months (range = 1 month-10 years). Reported symptoms included feeding intolerance (79%), emesis (64%), failure to thrive (43%), constipation (36%), and medically refractory reflux (29%). Prior therapies included anti-reflux medication in 11 patients (79%), multiple formula changes in 10 patients (71%), treatment for constipation in five patients (36%), and a promotility agent in one patient (7%). Nine patients (64%) were tolerating full oral feeds, while three (21%) required full or partial gastric feeds, and another three were receiving jejunal feeds. Sixty-four percent of patients had a history of being underweight (weight-for-age percentile <10), and the median preoperative weight-for-age percentile was 3.5. All patients had undergone an UGI study which was reported as negative for malrotation.
EF and intraoperative findings
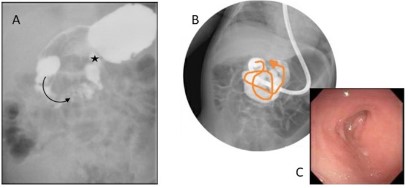
The most common finding documented on EF was a dilated duodenum just proximal to an area of luminal narrowing with associated caliber change (12/14 patients: 85.7%). Another 42.9% of patients (6/14) were found to have a “zig-zagging”, redundant, or tortuous duodenum (Figure 1). The differential diagnoses following EF included rotational abnormalities and partially obstructing Ladd’s bands, as well as possible annular pancreas or duodenal web. All patients were referred to general surgery for consideration of operative exploration and possible Ladd procedure. The study population included those patients that underwent a Ladd procedure for an intraoperative diagnosis of abnormal intestinal rotation with partially obstructing Ladd’s bands. One patient had a gastrostomy tube placed during the index operation as well.
Postoperative outcomes
Median postoperative hospital length of stay was 4 days (range = 2-105 days), with one patient remaining in the hospital for 105 days following a Ladd procedure due to an extended NICU stay that was not directly related to the patient’s index operation. Three patients (21.4%) were readmitted within 30 days after discharge, one for viral gastroenteritis, one for gastroparesis requiring addition of a promotility agent, and the last for acute segmental volvulus that required lysis of adhesions without bowel resection. There were no other documented postoperative complications.
Patient symptoms and weight trends were compared pre and postoperatively and are described in Table 2. Overall, there was a significant improvement in gastrointestinal symptoms following operative intervention, with 64% of patients having complete symptom resolution within 60 days post-operatively (100% of patients with documented symptoms preoperatively vs 36% postoperatively; p = 0.003). The most significant improvements were noted for symptoms of feeding intolerance (79% preoperatively vs 43% postoperatively; p = 0.02), failure to thrive (43% preoperatively vs 7% postoperatively; p = 0.03), and medically refractory reflux (29% preoperatively vs 0% postoperatively; p = 0.046). Though not a statistically significant increase, there was a trend toward improved tolerance of oral feeds with 64% of patients receiving full oral feeds preoperatively and 86% post-operatively (p = 0.08). Further, there was a significant increase in median weight-for-age percentiles from the 4th percentile pre-operatively to the 19th percentile by 60 days post-operatively (p = 0.01), and all 14 patients demonstrated an increase or plateau on the growth curve over the same period.
Table 1: Patient demographics and preoperative characteristics.
| Demographics and patient characteristics | All patients (N = 14) |
|---|---|
| Gender (% male) | 10 (71.4) |
| Race | |
| White/Caucasian | 8 (57.1) |
| Black/African American | 3 (21.3) |
| Hispanic/Latino | 1 (7.2) |
| American Indian | 1 (7.2) |
| Unknown | 1 (7.2) |
| Age at diagnosis (months); median [range] | 6.3 [3,156] |
| Gestational age at birth (weeks); median [range] | 39.5 [24,41] |
| Birth weight (kg); median [range] | 2.99 [0.66,3.6] |
| Presenting symptoms | |
| Feeding intolerance | 11 (78.6) |
| Emesis | 9 (64.3) |
| Failure to thrive | 6 (42.9) |
| Constipation | 5 (35.7) |
| Refractory reflux | 4 (28.6) |
| Duration of symptoms preoperatively (months); median [range] | 5.5 [1,120] |
| Receiving full PO feeds at diagnosis | 9 (64.3) |
| Preoperative weight-for-age percentile; median [range] |
3.5 [<1,33.6] |
| All numerical values displayed as no. (%) unless otherwise specified. Abbreviations: PO, per oral |
|
Table 2: Patient demographics and preoperative characteristics.
| Perioperative characteristics | Preoperative (N = 14) | Postoperative* (N = 14) | p-value |
|---|---|---|---|
| GI symptoms, any (% present) | 14 (100) | 5 (35.7) | 0.003m |
| Feeding intolerance | 11 (78.6) | 4 (28.6) | 0.02m |
| Emesis | 9 (64.3) | 5 (35.7) | 0.16m |
| Failure to thrive | 6 (42.9) | 1 (7.1) | 0.03m |
| Constipation | 5 (35.7) | 3 (21.4) | 0.32m |
| Refractory reflux | 4 (28.6) | 0 | 0.046m |
| Receiving full PO feeds | 9 (64.3) | 12 (85.7) | 0.08m |
| Weight-for-age percentile; median [range] | 3.5 [<1,33.6] | 19.4 [<1,63] | 0.01t |
All numerical values displayed as no. (%) unless otherwise specified.
Abbreviations: GI, gastrointestinal; PO, per oral
*Documented at last follow-up within 60 days postoperatively
Statistical tests: mMcNemar's test, tPaired t-test.
Discussion
This study introduces Endoscopic Fluoroscopy, a technique for the diagnosis of occult intestinal rotational abnormalities that is currently being used at our institution to identify patients that may benefit from a Ladd procedure. In our review of 14 patients who underwent a Ladd procedure following concern for abnormal rotation on EF, 64% of patients had complete symptom resolution by 60-days postoperatively and all patients demonstrated an increase or plateau on the growth curve over this same period. There were statistically significant improvements in GI symptoms postoperatively including feeding intolerance, failure to thrive, and medically refractory reflux, as well as a 5-fold increase in median weight-for-age percentile for the entire cohort. These findings demonstrate that EF is an effective tool for identifying patients with occult disorders of intestinal rotation that may benefit from a Ladd procedure in the setting of a negative or inconclusive UGI.
Fluoroscopic examination of the small intestine is not a novel technique as enteroclysis was introduced in the early 20th century to allow for improved small bowel imaging. The original enteroclysis technique involved placement of a balloon-tipped nasoduodenal tube followed by instillation of radiopaque contrast media, then insufflation with CO2 to distend the bowel and circumferentially coat the lumen with contrast [10]. This technique was used to identify small mucosal abnormalities as well as to assess the dynamics of the small bowel. However, with the advent of capsule endoscopy and improved axial imaging techniques, enteroclysis has not been as frequently utilized in recent years [11]. The benefits of EF over traditional enteroclysis include the ability to perform a focused examination of the proximal small intestine, provide direct visualization of the gastric and small bowel lumen, and permit the use of other diagnostic and therapeutic adjuncts such as mucosal biopsy or balloon dilation during the same procedure.
Pediatric patients with feeding intolerance and failure to thrive are often diagnostic dilemmas that undergo multitudes of diagnostic studies and invasive procedures with no definitive resolution. This study demonstrates EF to be an invaluable adjunct in the workup of these patients, especially in the setting of a negative or inconclusive UGI. Often, the volume of contrast instilled during fluoroscopic UGI is inadequate to evaluate for any luminal caliber change and may be significantly diluted by the time it reaches the distal duodenum, when the bowel is particularly tortuous. However, with direct instillation of contrast into the proximal duodenum there is less contrast dilution and a theoretically lower risk of aspiration, even in the setting of larger instillation volumes. Further, EF is performed by the gastroenterologist when upper endoscopy is indicated as part of the diagnostic workup, thereby eliminating the concern of additional anesthetic events.
There are certainly some recognized limitations of this study. The first lies in the retrospective, single-center design, as well as potential selection bias due to the narrow inclusion criteria. As this is a diagnostic technique being used by a single gastroenterologist at one institution and only as an adjunctive procedure in a specific patient population, the results are exploratory. However, patient selection was limited by available diagnostic and procedure codes, as well as the rarity of the underlying diagnosis. Extended follow-up of this patient cohort would be beneficial to assess the durability of the rotational abnormality diagnosis and subsequent operative intervention. Future prospective or randomized study of EF as a diagnostic technique is necessary to validate these results and evaluate the generalizability of the procedure.
This study describes a novel technique using Endoscopic fluoroscopy as an effective diagnostic tool for occult intestinal rotational abnormalities, which are often difficult to diagnose. EF provides three-dimensional visualization and dynamic assessment of the upper GI tract for this challenging clinical subset of patients. Once identification of these patients was possible, a Ladd procedure resulted in significant symptom resolution and universal improvement in growth parameters for this population. The findings outlined here demonstrate the utility of collaboration between the gastroenterologist and surgeon in patients with possible rotational abnormalities and inconclusive UGI imaging.
Declarations
Acknowledgements: None
Financial disclosures: Drs. Alyssa Mowrer, Christina Bence, Alfonso Martinez, and Amy Wagner have no conflicts of interest or financial ties to disclose.
References
- Brinkley MF, Tracy ET, Maxfield CM. Congenital duodenal obstruction: causes and imaging approach. Pediatr Radiol. 2016; 46: 1084-1095.
- Oelhafen K, Shayota BJ, Muhleman M, Klaassen Z, Shoja MM, et al. Peritoneal bands: A review of anatomical distribution and clinical implications. Am Surg. 2012; 78: 377-384.
- Prasil P, Flageole H, Shaw KS, Nguyen LT, Youssef S, et al. Should malrotation be treated differently according to age? J Pediatr Surg. 2000; 35: 756-758.
- Carroll AG, Kavanagh RG, Ni Leidhin C, Cullinan NM, Lavelle LP, et al. Comparative effectiveness of imaging modalities for the diagnosis of intestinal obstruction in neonates and infants: a critically appraised topic. Acad Radiol. 2016; 23: 559-568.
- Abdelwahed Y, Saber R, Imen BI, Hakim Z, Ayoub Z, et al. A case report of small bowel obstruction secondary to congenital peritoneal band in adult. Int J Surg Case Rep. 2017; 30: 23-25.
- Akgur FM, Tanyel FC, Buyukpamukcu N, Hiçsönmez A. Anomalous bands causing intestinal obstruction in children. J Pediatr Surg. 1992; 27: 471-473.
- Etensel B, Ozkisacik S, Doger F, Yazici M, Gürsoy H, et al. Anomalous congenital band: a rare cause of intestinal obstruction and failure to thrive. Pediatr Surg Int. 2005; 21: 1018-1020.
- Kassem MW, Patel M, Iwanaga J, Loukas M, Tubbs RS, et al. Constriction of the stomach by an unusual peritoneal band. Cureus. 2018; 10: e2148.
- Mazziotti MV, Strasberg SM, Langer JC. Intestinal rotation abnormalities without volvulus: the role of laparoscopy. J Am Coll Surg. 1997; 185: 172-176.
- Maglinte DD, Kohli MD, Romano S, Lappas JC. Air (CO2) double-contrast barium enteroclysis. Radiology. 2009; 252: 633-641.
- Maataoui A, Vogl TJ, Jacobi V, Jacobi V, Khan MF. Enteroclysis: Current clinical value. World J Radiol. 2013; 5: 253-258.