Journal of Gastroenterology Research and Practice
Case Report - Open Access, Volume 3
MPOX: Typical lesions in unusual places
Zuchen Flavia; Lima João PV; Deriquehem Vitor AS; Goulart Bruno S; Caramenez Erika A; Moraes Antonio CS*
Internal Medicine Department Hospital Copa D’or, Private hospital in Rio de Janeiro, Brazil.
*Corresponding Author : Antonio Carlos de Moraes
Internal Medicine Department Hospital Copa D’or,
Private Hospital in Rio de Janeiro, Brazil.
Tel: +55-21-999549061;
Email: antonio.moraes@copador.com.br
Received : Feb 28, 2023
Accepted : Apr 14, 2023
Published : Apr 21, 2023
Archived : www.jjgastro.com
Copyright : © Antonio Carlos DM (2023).
Abstract
A 54-year-old man seeks the Emergency Room due to a three-day course of left flank and left iliac pain. He had a past medical history of type 2 diabetes mellitus and splenectomy seven years ago. He denied fever and showed no signs of bowel obstruction. Pain was worsened upon palpation of the left quadrants. Digital rectal exam was unremarkable and there were no skin or ocular lesions on the physical exam.
A Computerized Tomography (CT) scan of abdomen and pelvis was performed, showing significant parietal thickening of the lower rectum, with densification of meso-rectal fat and adjacent lymph nodes enlargement. Complete blood count and comprehensive metabolic panel were unremarkable. Patient had an increased C-reactive protein. He was admitted for pain management and further investigation. Inflammatory Bowel Disease (IBD) and Infectious Colitis were suspected.
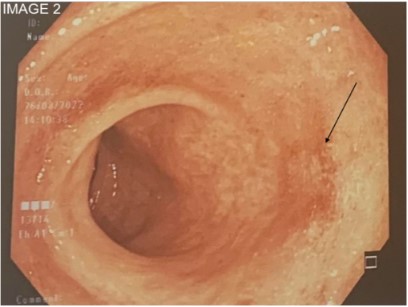
A colonoscopy was performed on the third day of admission. Mucosa was enanthematous and friable. There was loss of the usual vascular pattern and numerous punctate, shallow, fibrinous bottom, flat edge erosions. Some were confluent, distributed circumferentially in the distal 10 centimeters of the rectum. The findings were suggestive of Mpox (formerly known as monkeypox), later confirmed by biopsy. Patient had monogamous receptive anal intercourse and HIV testing was negative.
The referred case is unusual because of the lack of skin lesions during the course of the disease. It is the most common clinical finding, achieving an incidence of 100% in some studies [1,2]. It is expected to appear early, around the second and third day after systemic symptoms start [3]. Patient was hospitalized and observed during the early symptoms until resolution. It is an atypical presentation of Mpox with colitis as its unique finding.
Keywords: Monkeypox; Mpox; Global emergency.
Citation: Flavia Z, Lima João PV, Deriquehem Vitor AS, Caramenez Erika A, Moraes Antonio CS, et al. MPOX: Typical lesions in unusual places. J Gastroenterol Res Pract. 2023; 3(3): 1137.
Introduction
Mpox, originally known as monkeypox, is named similarly to smallpox because of its close clinical presentation, though less severe than the former. It is caused by an enveloped double-stranded DNA virus of the Poxviridae family, being firstly identified in 1970 in the African continent and since then it has become endemic to the area. It started as a zoonotic infection before the human-to-human transmission. Can be carried in secretions, contaminated objects and respiratory droplets [2].
Epidemiological findings suggest that men are more likely to contract the virus, the most vulnerable cluster of them being men who have sex with men [4], most having the usual self-limited disease course of two to four weeks [3]. Fatal cases are more present in children under the age of twelve and immuno-compromised adults [5].
The typical clinical presentation starts after an incubation period of one to two weeks [2] with fever, fatigue, headache and other nonspecific symptoms of systemic illness lasting five days. Then, it becomes more distinct with synchronic evolving rash, affecting mucous membranes, external genitalia and the cornea [2-5]. The rate of perceivable rash in clinical examination can be as high as 100% [1]. Another common finding is lymph-adenopathy [2-5]. Clinical suspicion indicates confirmation testing using methods such as Polymerase Chain Reaction (PCR) of swab samples of the lesions. Sequelae is most common in those unvaccinated and can include blindness [3,5].
Currently, the main antiviral treatment is tecovirimat, indicated for high risk patients of severe disease [6], making supportive care the main choice for all patients. Prevention remains the most valuable way to face mpox, since vaccination is not widely available [2]. The first outbreak outside Africa was in 2003, and the largest worldwide outbreak started in 2022 [2]. Thus far in 2023, the world has had over 85000 confirmed cases with 93 deaths, all in high risk people [7]. It is considered a Public Health Emergency of International Concern (PHEIC) by the World Health Organization (WHO) [7].
Materials and methods
Case report of a patient admitted in a tertiary hospital in September 2022.
Results
A 54 year-old latin american man presented to the Emergency Room with a three day history of continuous diffuse abdominal pain, worst on the left flank and left iliac region. He denied changes in his bowel transit, fever and systemic symptoms. He had a past medical history of type 2 diabetes and splenectomy due to splenic vein thrombosis five years ago. He took metformin daily. Social history showed regular receptive anal intercourse with the same partner for a couple of months without use of preservatives. He denied drug allergies and there were no remarkable diseases in his family.
Physical examination had no alterations besides worsening pain with deep palpation in the referred areas. Cell blood count and comprehensive metabolic panel were normal, only C-reactive protein was increased. A Computerized Tomography scan (Figure 1) presented significant parietal thickening of the lower rectum, with densification of mesorectal fat and adjacent lymph nodes enlargement. He was admitted for further investigation and pain management. Inflammatory bowel disease and infective colitis were initially suspected.
Colonoscopy (Figure 2) was performed and found an enanthematous, friable mucosa. There was loss of the usual vascular pattern, with numerous punctate, shallow, fibrinous bottom, flat edges erosions. Some were confluent, distributed circumferentially in the distal 10 centimeters of the rectum. A dry swab confirmed the diagnosis of Mpox. HIV, chlamydia and gonorrhea testing were negative.
Patient had mild symptoms and supportive care improved his clinical status. He was discharged after four days of symptomatic treatment, with outpatient follow up with resolution of symptoms.
Discussion
Patient presented an unusual Mpox case with no other symptom rather than abdominal pain. Laboratory had only an inflammatory increase and CT scan presented unspecific signs of colitis. Even though digital rectal exam and serial dermatological examinations were performed, there were no clinical findings of Mpox, requiring an invasive exam. The main clinical hypotheses were inflammatory bowel disease and infective colitis. At the colonoscopy, it was possible to see the classic lesions concealed to the physical exam. Colonoscopist justified the search for Mpox because of the endemic infections and active history of receptive sexual intercourse.
Conclusion
It is important to keep Mpox as an up to date differential diagnosis of proctitis, even without classical skin lesions or systemic symptoms. Though most cases are self limited, the diagnosis is crucial to make sure the disease is restrained from further dissemination and identify risk groups for more aggressive progression to receive proper care
References
- Epidemiological and Clinical Characteristics of Monkeypox Cases-United States Center for Disease Control and Prevention, 2022.
- Monkeypox. World Health Organization, 2022.
- Guidance on Clinical Suspicion and Differential Diagnosis of Monkeypox. Pan American Health Organization, 2022.
- Monkeypox. The New England Journal of Medicine, 2022.
- Clinical Management and Infection Prevention and Control for Monkeypox. World Health Organization, 2022.
- Guidance for Tecovirimat Use. Centers for Disease Contol and Prevention, 2022.
- Multi-Country Outbreak of Mpox. World Health Organization, 2023.