Journal of Gastroenterology Research and Practice
Research Article - Open Access, Volume 3
Initial results of screening program in Mongolia where burdening high gastric cancer
Jargalsaikhan Bilguun1; Khurelbaatar Tsevelnorov2; Tserenchimed Sarantuya3; Khasag Oyuntsetseg2; Duger Davaadorj1,2; Tsogt-Ochir Byambajav1,2; Tuvshinbaigal Amarmend3; Sangidaansuren Orkhontuya4; Shirbazar Lhamsuren5; Purevjav Myagmarsuren6; Altanhuyag Bayarjargal7; Byambasuren Khaliun8; Sukhbaatar Alimaa9; Boldbaatar Gantuya1,3*
1Department of Gastroenterology, School of Medicine, Mongolian National University of Medical Sciences (MNUMS), Ulaan- baatar city, Mongolia.
2Endoscopy Unit, Mongolia Japan Hospital of MNUMS, Ulaanbaatar City, Mongolia.
3Endoscopy Unit, Intermed hospital, Ulaanbaatar City, Mongolia.
4Chinmend Hospital, Uvurkhangai Province, Mongolia.
5General Hospital of Gobi-Altai province, Mongolia.
6General Hospital of Dundgobi province, Mongolia.
7Regional Diagnostic and Treatment Center of Dornod Province, Mongolia.
8Adistat Nar Hospital, Ulaanbaatar City, Mongolia.
9Mungunguur Hospital, Ulaanbaatar City, Mongolia.
*Corresponding Author : Boldbaatar Gantuya
Ulaanbaatar city, Botanical street, Mongolian National
University of Medical Sciences, Mongolia.
Email: gantuya@mnums.edu.mn
Received : Feb 27, 2023
Accepted : Apr 10, 2023
Published : Apr 17, 2023
Archived : www.jjgastro.com
Copyright : © Gantuya B (2023).
Abstract
Background: Mongolia is the leading country by the incidence and mortality rate of gastric cancer. In 2022 national cancer screening program for upper gastrointestinal neoplasia was initiated therefore we conducted the multi-center study for determining the gastric cancer among Mongolian population.
Methods: The cross-sectional study was performed to examine the detection rate of gastric cancer cases based on national screening program from May to September in 2022. The primary outcomes of this study was to define detection rate (proportion of positive cases among individuals who underwent endoscopic screening) and to determine the characteristics of cancer type including its precursor disease based on histological examination.
Results: Totally 34,581 people were screened in the 28 endoscopy centers. Among them n=262 (0.8%) patients diagnosed with gastric cancer based on endoscopic examination. The proportion of early stage gastric cancer was n=135 (51.5%) of all screened cancer cases.
Conclusion: The initiation of Mongolian national gastric cancer screening program was useful to detect gastric cancer in early stage which further can reduce mortality rate of gastric cancer due to its treatment possibilities. Therefore, national screening program should be continuous.
Keywords: Gastric cancer; Screening program; Mongolia.
Abbreviations: LGD: Low Grade Dysplasia; HGD: High Grade Dysplasia; EGC: Early Gastric Cancer; AGC: Advanced Gastric Cancer.
Citation: Bilguun J, Tsevelnorov K, Sarantuya T, Oyuntsetseg K, Davaadorj D, et al. Initial results of screening program in Mongolia where burdening high gasric cancer. J Gastroenterol Res Pract. 2022; 3(2): 1136.
Introduction
The most recent GLOBOCAN report estimated a total of 1,089,103 incident cases and 768,793 deaths due to gastric cancer in 2020 [1]. Globally, gastric cancer is one of the most common malignancies, accounting for more than 1 million cases per year and 5.7% of all cancer diagnoses [2]. The 5-year survival prognosis is poor because the majority of cases present with distant or distant metastases. Gastric cancer incidence is 5-20 times higher than the average in East Asian countries, depending on the geographical area [3]. High-risk regions include Asia with the highest incidence rates in several Asian countries, especially Mongolia, Japan, Korea and China [4]. The reason for this geographical variation remains elusive, but may correlate with the incidences of Helicobacter pylori (H. pylori) infection, smoking, and the consumption of salt and salt-preserved foods [5].
For Mongolians, the incidence and age-adjusted cancer mortality rates for gastric is the highest in the Asia-Pacific region [6], and this is due to poor survival or prognosis due to late-stage diagnosis and limited quality of health services [7]. In Mongolia, since the mid-1960s, a hospital-based cancer registry data-base was established at the National Cancer Research Center, and the quality of cancer registry data has been maintained at a good level since the information was released from the center [8].
For the future trend although the age-standardized rates of GC in most countries have declined including China, Japan, South Korea, and Mongolia until 2030, but the absolute deaths would still increase significantly, especially in South Korea and Mongolia based on Bayesian age-period-cohort model application [9]. It might be because of low socio-demographic index and aging along with H. pylori infection, smoking, and high-salt diet were the main risk factors of gastric cancer occurrence [9].
H. pylori infection was the major gastric health problem among the Mongolian population that the H. pylori infection was high in all parts of Mongolia, with an overall infection rate was 70-80%. In addition, environmental factors such as high salt intake worsened the clinical outcome [10].
According to the national health indicator data, TNM stage at the time of cancer diagnosis, gastric cancer diagnosis is 0.4% in the carcinoma in-situ stage, 5.1% in stage I, 15.2% in stage II, 42.7% in stage III and 36.5% in stage IV 36.5 % were diagnosed respectively. In Mongolia most of the diagnoses of gastric cancer are in the late stage. Therefore, early diagnosis of gastric cancer with its appropriate treatment choice such as endoscopic submucosal dissection and or partial gastrectomy are the beneficial for the future prognosis.
The Government of Mongolia and the Ministry of Health provided screening program based on national major risk factors for communicable and non-communicable diseases including cancer screening in 2022. In Mongolia, there is a lack of data for gastric cancer screening. Endoscopic screening program have been started on May 1, 2022 across Mongolia to diagnose upper gastrointestinal tract cancer in a representative population over 35 years old. Therefore, we conducted the multi-center study for determining the gastric cancer and its background diseases among Mongolian population in the initial period of screening survey.
Materials and methods
TThe research was carried out in accordance with the principles of the “International Biomedical Research Ethical Guidelines” and the topics, methods and methods approved by the Declaration of Helsinki and the decision of the Ethical Subcommittee of the AUSU.
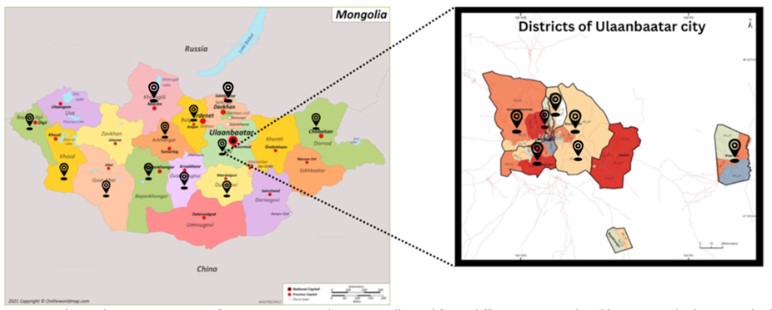
We conducted cross sectional study based on Mongolian nationwide endoscopic screening program among above 35-year-old peoples. We collected data from 28 endoscopy centers from the Ulaanbaatar city, western part (Bayan-Ulgii, GoviAltai, Hovd), eastern part (Dornod), southern part (Dundgovi, Bayankhongor), northern part (Khuvsgul, Orkhon, Selenge) and central part (Arkhangai, Uvurkhangai) of Mongolia from May to September in 2022. The data collection from different geographical locations are described in Figure 1.
The primary outcomes of this study was to determine the incidence rate of gastric cancer based on endoscopic diagnosis. Further the secondary outcome of the research among detected gastric cancer patients, the distribution of cancer type was based on histopathological examination. The histological criteria for gastric cancer and its precursor diseases was based on using WHO guidelines classification, gastric cancer can be classified as adenocarcinoma (including dysplasia high grade, poorly cohesive and tubular adenocarcinoma, well, moderate, poor differentiated adenocarcinoma), signet ring-cell carcinoma, and undifferentiated carcinoma. Low grade dysplasia and atypical cells are classified as the precursor diseases.
We used appropriate statistical methods in STATA software. We calculated mathematical mean M, 95% confidence interval (CI 95%) center limit of activity and the relationship between the diagnosis percentation and quantitative indicators of endoscopic macro changes was determined by one-way table.
Results
Totally 34581 participants data were collected from 28 endoscopy centers from Ulaanbaatar city and province hospitals. The age range of the study participants was 35 to 93 years old. In terms of gender, 56.8% are men and 43.13% are women. The mean with SD age of people diagnosed with gastric cancer was 61.56 ± 1.11, while the mean with SD age of healthy people was 53.84 ± 0.29 (p value 0.0001).
Among them 262 (0.8%) patients diagnosed with gastric cancer based on endoscopic examination. The proportion of suspected early stage gastric cancer cases was n=135 (51.5%) based on endoscopic examination.
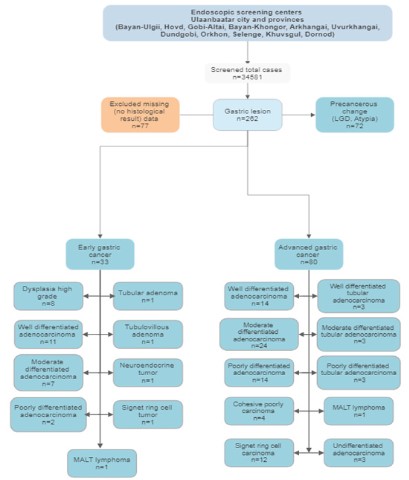
Final diagnosis was confirmed by histological evaluation. Among gastric cancer suspected screened 262 cases, 77 cases were excluded because of lacking histological evaluation. In the remaining 185 cases histological examination was performed. The n=113 (61.1%) of them diagnosed as the gastric cancer. The remaining n=72 (38.9%) cases was precursor gastric cancer diseases. Overall case series is shown in Figure 2 and Table 1 more in detail.
Table 1: Cancer screening result.
| (%) | (N) Cases ases | ||
|---|---|---|---|
| Gastric cancer cases based on endoscopic examination (Total case n=34581) | |||
| Non-gastric cancer cases | 99.20% | 34319 | |
| Gastric cancer suspected cases | 0.80% | 262 | |
| Proportion of early and advanced gastric cancer (n=262) | |||
| Early gastric cancer | 51.50% | 135 | |
| Advanced gastric cancer | 48.50% | 127 | |
| Histological result of total cases (n=185) | |||
| Gastric cancer | Dysplasia high grade | 4.30% | 8 |
| Well differentiated adenocarcinoma | 13.50% | 25 | |
| Moderate differentiated adenocarcinoma | 16.80% | 31 | |
| Poorly differentiated adenocarcinoma | 8.60% | 16 | |
| Cohesive poorly carcinoma | 2.20% | 4 | |
| Tubular adenoma | 0.50% | 1 | |
| Tubulovillous adenoma | 0.50% | 1 | |
| Well differentiated Tubular adenocarcinoma | 1.70% | 3 | |
| Moderate differentiated Tubular adenocarcinoma | 1.70% | 3 | |
| Poorly differentiated Tubular adenocarcinoma | 1.10% | 2 | |
| Neuroendocrine tumor | 0.50% | 1 | |
| Signet cell tumor | 7.00% | 13 | |
| MALT lymphoma | 1.10% | 2 | |
| Undifferentiated adenocarcinoma | 1.70% | 3 | |
| Precursor lesion | Dysplasia low grade | 37.80% | 70 |
| Atypical cells | 1.10% | 2 | |
Discussion
Gastric cancer remains one of the most common and dead- ly diseases in Mongolia. There are generally no early signs or symptoms of stomach cancer and it contains a poor prognosis because almost 80% of cases are diagnosed in the late stage [6-8]. Therefore, effective management of the prevention, early detection, and treatment of stomach cancer is important to reduce the mortality. Countries, such as, South Korea, Japan have high incidence of stomach cancer but have a low mortality rate due to the implementation of national evidence-based prevention and early detection program for stomach cancer [11-15].
The age standardized incidence of gastric cancer in Mongolia (32.5 in 100,000 populations) is almost similar to Japan (31.6) however its mortality rate in Japan (8.2) is far fewer than in Mongolia (24.6). In Mongolia, more than 80% of people diagnosed with late-stage of gastric cancer, which results in higher mortality rates [6-8]. In the other hand almost 80% of people diagnosed with early-stage of gastric cancer among Japanese and Korean where national cancer screening programs initiated for several decades [16-18].
According to the Japanese studies where endoscopic examinations were introduced, the gastric cancer detection rate was 0.30-0.87% for gastroscopic examinations [19,20] and the proportion of early-stage cancer was approximately 80% in the endoscopic screening group which can reduce mortality rate by 40% for gastric cancer [18,21]. Gastric cancer screening by endoscopy testing through the National Cancer Screening Program of Korean study showed that the detection rates of gastric cancer by endoscopy in the first and subsequent rounds were 2.71 and 2.14 per 1000 examinations, respectively [22].
In this study Mongolian national gastric cancer screening program showed that the overall gastric cancer detection rate was the 0.8% and the proportion of early stage gastric cancer was 51.5% based on endoscopic examination which was shown the beneficial effect than those period of without screening program (20% vs 51.5%) [6-8]. In other words, because of national screening program, the early stage gastric cancer detection rate was improved 2.5 times that those patients having chance to eradicate the cancer based on endoscopic submucosal dissection or surgical interventions. However, comparing with Japan and Korea where having the high incidence of gastric cancer area Mongolian early stage gastric cancer detection rate is still in the lower range. Therefore, quality of the endoscopic examination may need to be more improved.
Despite incidence and mortality rate of gastric cancer declining global trends, gastric cancer remains an important cause of cancer mortality contributing to 8% of all cancer-related deaths in 2020. Whilst screening strategies are important for early detection in high-risk populations, the reduction in prevalence of H. pylori infection as well as the reduction in other known risk factors is key to prevention of gastric cancer [23,24]. Screening can detect early and late stage tumors and increase the effectiveness of their treatment. Therefore, it is desirable to increase the coverage of screening tests, to maintain a high level of communication and hierarchy between hospitals, and to further improve the effectiveness of cancer diagnosis and treatment.
Conclusion
The initiation of Mongolian national gastric cancer screening program was useful to detect gastric cancer in early stage. Therefore, national screening program should be continuous.
Declarations
Conflicts of interest: No conflicts of interest.
Funding sources: Not applicable.
Acknowledgements: We would like to acknowledge our sincere gratitude for following doctors who sharing their valuable screening data: B. Amgalan-General hospital of Arkhangai province, M.Dariimaa-General hospital of Uvurkhangai province, L. Aigul-General hospital of Bayan-Ulgii province, B. Enkhjargal-Regional diagnostic and treatment center of Khovd province, J.Dulmaa-General hospital of Bayankhongor province, Yo. Suvd-Erdene, G. Shagdarsuren-Regional diagnostic and treatment center of Orkhon province, Z. Bolormaa-Erdenet medical hospital, B.Bud-General Hospital of State Special Employees, S.Roza-Citymed hospital, O.Tseveendari-Shastin state 3rd hospital, Ts.Chanchaldulam-General hospital of Baganuur district, Ts.Bayarjargal-Ulaanbaatar Railway General Hospital, G. Sergelen-Shinonmed hospital, B.Bolortuya-Health center of Songino Khairkhan District, O.Munkhsaikhan-Express diagnostic center, Azzaya-Mon-medical hospital, D. Munkhgerel-Ireedui hospital.
Research implementation support organization: It was carried out under the supervision of B. Gantuya, a lecturer of the Department of Gastrointestinal Departmet of Mongolian National University of Medical Science and Ts.Sarantuya, Intermed hospital. We collected data from 28 endoscopy centers authorized to carry out endoscopy screening program supported by governmental health insurance system.
References
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021; 71: 209-249.
- Rawla P, Barsouk A. Epidemiology of gastric cancer: global trends, risk factors and prevention. Prz Gastroenterol. 2019; 14: 26-38.
- Sitarz R, Skierucha M, Mielko J, Offerhaus GJA, Maciejewski R, et al. Gastric cancer: epidemiology, prevention, classification, and treatment. Cancer Manag Res. 2018; 10: 239-248.
- Ning FL, Lyu J, Pei JP, Gu WJ, Zhang NN, et al. The burden and trend of gastric cancer and possible risk factors in five Asian countries from 1990 to 2019. Sci Rep. 2022; 12: 5980.
- Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F, et al. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomarkers Prev. 2014; 23: 700-713.
- Chimed T, Sandagdorj T, Znaor A, Laversanne M, Tseveen B, et al. Cancer incidence and cancer control in Mongolia: Results from the National Cancer Registry 2008-12. Int J Cancer. 2017; 140: 302-309.
- Sandagdorj T, Sanjaajamts E, Tudev U, Oyunchimeg D, Ochir C, et al. Cancer incidence and mortality in Mongolia - National Registry Data. Asian Pac J Cancer Prev. 2010; 11: 1509-14.
- Lonjid T, Sambuu T, Tumurbat N, Banzragch U, Dondov G, et al. Incidence of Stomach and Esophageal Cancers in Mongolia: Data from 2009 to 2018. Euroasian J Hepatogastroenterol 2020;10:16-21.
- Yang X, Zhang T, Zhang H, Sang S, Chen H, et al. Temporal trend of gastric cancer burden along with its risk factors in China from 1990 to 2019, and projections until 2030: comparison with Japan, South Korea, and Mongolia. Biomark Res. 2021; 9: 84.
- Khasag O, Boldbaatar G, Tegshee T, Duger D, Dashdorj A, et al. The prevalence of Helicobacter pylori infection and other risk factors among Mongolian dyspeptic patients who have a high incidence and mortality rate of gastric cancer. Gut Pathog. 2018; 10: 14.
- Hamashima C. Systematic Review G, Guideline Development Group for Gastric Cancer Screening G. Update version of the Japanese Guidelines for Gastric Cancer Screening. Jpn J Clin Oncol. 2018; 48: 673-683.
- Kim B, Cho SJ. Endoscopic Screening and Surveillance for Gastric Cancer. Gastrointest Endosc Clin N Am. 2021; 31: 489-501.
- Lu YF, Liu ZC, Li ZH, Ma WH, Wang FR, et al. Esophageal/gastric cancer screening in high-risk populations in Henan Province, China. Asian Pac J Cancer Prev. 2014; 15: 1419-1422.
- Mabe K, Inoue K, Kamada T, Kato K, Kato M, et al. Endoscopic screening for gastric cancer in Japan: Current status and future perspectives. Dig Endosc. 2022; 34: 412-419.
- Zeng H, Sun K, Cao M, Zheng R, Sun X, et al. Initial results from a multi-center population-based cluster randomized trial of esophageal and gastric cancer screening in China. BMC Gastroenterol. 2020; 20: 398.
- Lee S, Jun JK, Suh M, Park B, Noh DK, et al. Gastric cancer screening uptake trends in Korea: results for the National Cancer Screening Program from 2002 to 2011: a prospective cross-sectional study. Medicine (Baltimore). 2015; 94: e533.
- Nakamura Y, Takeshita M, Hirota Y, Ueda K, Yao T, et al. An evaluation of gastric cancer screening program in Hisayama, Japan. Gastroenterol Jpn. 1977; 12: 427-34.
- Yashima K, Shabana M, Kurumi H, Kawaguchi K, Isomoto H, et al. Gastric Cancer Screening in Japan: A Narrative Review. J Clin Med. 2022; 11.
- Hamashima C, Fukao A. Quality assurance manual of endoscopic screening for gastric cancer in Japanese communities. Jpn J Clin Oncol. 2016; 46: 1053-1061.
- Sugano K. Screening of gastric cancer in Asia. Best Pract Res Clin Gastroenterol. 2015; 29: 895-905.
- Zhang X, Li M, Chen S, Hu J, Guo Q, et al. Endoscopic Screening in Asian Countries Is Associated With Reduced Gastric Cancer Mortality: A Meta-analysis and Systematic Review. Gastroenterology. 2018; 155: 347-354 e9.
- Choi KS, Jun JK, Lee HY, Park S, Jung KW, et al. Performance of gastric cancer screening by endoscopy testing through the National Cancer Screening Program of Korea. Cancer Sci 2011; 102: 1559-1564.
- Arnold M, Park JY, Camargo MC, Lunet N, Forman D, et al. Is gastric cancer becoming a rare disease? A global assessment of predicted incidence trends to 2035. Gut. 2020; 69: 823-829.
- Morgan E, Arnold M, Camargo MC, Gini A, Kunzmann AT, et al. The current and future incidence and mortality of gastric cancer in 185 countries, 2020-40: A population-based modelling study. EClinicalMedicine. 2022; 47: 101404.