Journal of Gastroenterology Research and Practice
Case Report - Open Access, Volume 3
A rare case of serous cyst adenocarcinoma of pancreas with splenic tuberculosis and neuro endocrine deposits in omentum of a young female
Mukesh Kalla1; Komal Kalla2; Menka Kapil3*; Ganesh Agarwal4; Alok Verma5; Aman Manocha6; Anuj Sharma3
1Chief Gastroenterologist, S R Kalla Memorial Gastro and General Hospital, Jaipur, India.
2Chief Histopathologist, S R Kalla Memorial Gastro and General Hospital, Jaipur, India.
3Consultant Pathologists, S R Kalla Memorial Gastro and General Hospital, Jaipur, India.
4Consultant Surgeon, S R Kalla Memorial Gastro and General Hospital, Jaipur, India.
5Consultant Anaesthesiologist, S R Kalla Memorial Gastro and General Hospital, Jaipur, India.
6Consultant Radiologist, S R Kalla Memorial Gastro and General Hospital, Jaipur, India.
*Corresponding Author : Menka Kapil
Consultant Pathologists, S R Kalla Memorial
Gastro and General Hospital, Jaipur, India.
Email: drmenkapath@yahoo.com
Received : Feb 04, 2023
Accepted : Mar 07, 2023
Published : Mar 14, 2023
Archived : www.jjgastro.com
Copyright : © Kapil M (2023).
Abstract
Cystic tumours of pancreas with malignant potential are very rare including serous cystic tumour, although mucinous cystic neoplasms of pancreas possess more frequent ability to transmute into mucinous cystadenocarcinoma. Neuroendocrine Tumors (NETs) are rare tumors comprising approximately 2% of all malignancies. The most common sites are gastrointestinal tract and the lung. Most of these tumors are well-differentiated and have an indolent course therefore an incidental finding.
Tuberculosis remains one of the most prevalent and fatal infectious diseases in spite of continuous efforts to efface it. It is a multi-systemic disease. Pulmonary tuberculosis is the most common manifestation however extra pulmonary disease accounts for almost 15-20% of all tuberculosis.
We are presenting an extremely rare case of a young female with diagnosis of triple pathologies including serous cyst adenocarcinoma pancreas a rare finding, with tuberculosis of spleen and neuroendocrine deposits in omentum at our tertiary care hospital of Gastroenterology. After extensive search of literature on PubMed and Medline we did not find any case resembling such findings of pathologies thus it might be the first case of world with triple pathologies in a young female patient at the age of 28 years.
Keywords: Serous cyst adenocarcinoma pancreas; Tuberculosis; Neuroendocrine tumour.
Citation: Kalla M, Kalla K, Kapil M, Agarwal G, Verma A, et al. A rare case of serous cyst adenocarcinoma of pancreas with splenic tuberculosis and neuro endocrine deposits in omentum of a young female. J Gastroenterol Res Pract. 2023; 3(1): 1130.
Introduction
Cystic neoplasms of the pancreas with malignant potential are very rare and comprises only of 1-2% of all exocrine pancreatic malignancy [1,2]. In 1978, Compagno and Oertel [3] gave histopathologic classification of cystic neoplasms of the pancreas according to their different biological behavior. The neoplastic cysts of Pancreas are classified as serous and mucinous [4]. The serous cystic neoplasm classified as benign serous cystadenoma and cystadenocarcinoma the malignant lesion which is rare but known malignant condition also described in the literature. Mucinous cystic neoplasms of pancreas carry more frequent ability to convert to its malignant counterpart mucinous cystadenocarcinoma [5]. Serous cystadenocarcinoma is extremely rare and the case reports established the age to be in elderly but in our case the patient was young female of twenty-eight years.
Neuroendocrine Tumor (NET) is a rare type of tumor that arises from specialized body cells called neuroendocrine cells. These cells have traits of both nerve cells and hormone-producing cells.The diagnosis of NET mainly relies on the positive assessment of markers of neuroendocrine differentiation by immunohistochemistry [6,7]. The most commonly used markers are general neuroendocrine markers either in the cytosol such as neuron-specific enolase (NSE) and the protein gene product 9.5 or granular markers such as chromogranin A (CgA) and synaptophysin [8]. Splenic tuberculosis is extremely rare and has no characteristic symptoms or abnormal imaging findings. Therefore, it is likely to be misdiagnosed as carcinoma of spleen, splenic abscess, lymphoma, rheumatic fever. There are no specific symptoms for establishing the diagnosis of splenic TB [8] In our case the patient had only symptom of abdominal pain with high ESR.
Case report
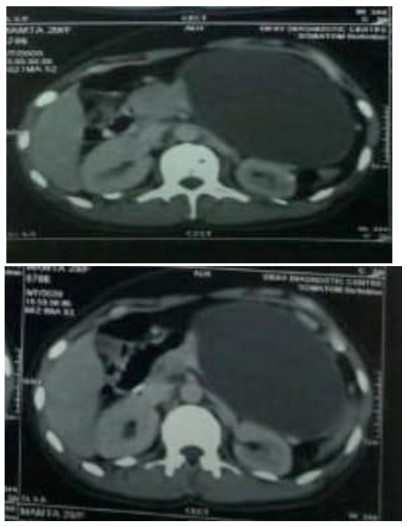
We report a case of 28 years old female suffering from acute upper abdominal pain since one year and was not able to get proper treatment and reffered to our hospital. With complaint of abdominal pain she was admitted to a hospital near by her home, where she was investigated and had imaging finding of CECT abdomen which was likely in favour of pancreatic cyst possibly peudocyst formation with feature of collection of fluid. Few ill defined, hypoenhancing, hypoattenuating areas in splenic parenchyma on anterio superior aspect were seen and advised for further evaluation. There she had undergone for aspiration of fluid approximately 580 ml pus was aspirated from cyst of pancreas and then after she was discharged from that hospital. After two months again she developed abdominal pain with discomfort and admitted to our hospital.
The patient at our hospital was extensively investigated for further diagnois and management of continuous abdominal pain. She had no previous chronic illness and no history of surgery. She had no past medical history of hypertension, diabetes mellitus, coronary heart disease. Her complete blood counts revealed wbc-5000/cumm, hemoglobin-9.1 gm%, platelets-1.80 lakh/cumm. With peripheral blood examination showed microcytic hypochromic picture with no immature cell and no hemoparasite. Her PT and INR values were normal. Liver function test showed Amylase 20.9 U/l, lipase 128.6 U/L, Total Bilirubin 0.62mg/dl, Total Protein 6.7 g/dl, SGOT 151 U/L and SGPT 52.7 U/L. Renal function test with Creatinine 1.0 mg/dl, blood urea 17 mg/dl were also within normal range. HbS antigen was negative and HIV antibodies were non-reactive. Her CA 19-9 was 82.65 U/ml which was high.
On imaging studies at our hospital, CT of chest had no specific abnormality while CT abdomen showed very large well defined encapsulated cystic lesion measuring 10.4 x 9.2 x 11.2 in region of body and tail of pancreas with mild splaying of pancreatic tissue in body region. Fluid attenuation contents were seen with tiny mural nodule along inferior surface of the cyst. Surrounding fat planes were intact, reteropancreatic splenic vein was attenuated with multiple collaterals in gastrosplenic ligament and perigastric lesion along superior and lateral aspect of cyst. Spleen showed mild splenomegaly with few small hypodense areas along superior and mid lower pole small infarcts, few small retroperitoneal and mesenteric lymph nodes were seen.
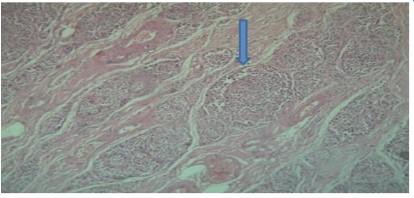
As the cystic lesion was very large so patient underwent for surgery, operative exploration revealed a large firm cystic mass Figure 3 from tail to head of pancreas reaching up to spleen. Pancreatectomy and splenectomy was done. The pancreas, spleen, omental tissue were sent to histopathology laboratory.
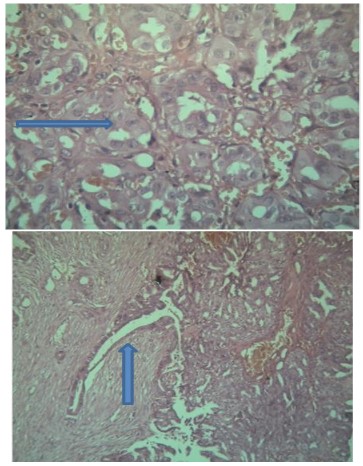
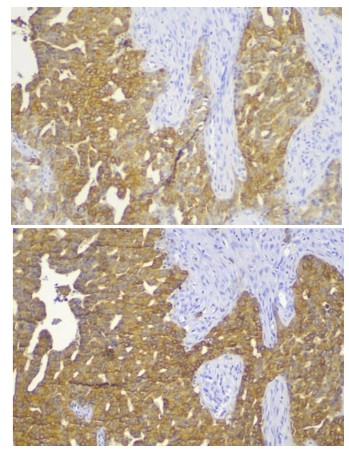
The gross cystic mass measures 10 x 7 x 5 cms, external surface was bosselated irregular with congestion, the normal pancreatic tissue was pushed to the periphery. The cyst was sectioned to reveal tan and red variegated cystic and solid cut surfaces. Microscopic examination demonstrated cystic wall lined by glycogen rich clear cells arranged in a single cuboidal layer without mucin. The Linning epithelial cells demonstrate high grade of dysplasia and foci of microinvasive adenocarcinoma. Perineural and lymphovascular invasion were not identfied. Immunohistochemistry was performed for further confirmation which showed CK-7, CK- 19, CA19.9 positive while CK-20, CDX-2, CEA were negative thus diagnosis of serous cystadenocarcinoma was confirmed.
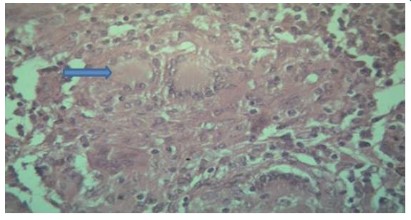
The other specimen received was of spleen which measures 12.6 x .5 x 2.5 cms with external surface congested and few grey white firm nodular areas, cut section showed red pulp and white pulp with few grey white irregular areas. Splenic hilum was identified. On microscopy from multiple sections from spleen show features of chronic venous congestion along with presence of multiple epitheloid cell granuloma with caseous necrosis and multiple langhans giant cell suggestive of tuberculosis which was incidental finding and patient had only abdominal pain metastases but tubercular lesion was very challenging to report and no other symptoms related to tuberculosis as if anorexia, fever, weight loss. Polymerase chain reaction for tuberculosis came positive which was confirmatory to support our diagnosis No foci of any metastases to spleen was noted, tubercular lesion was very challenging to report in this case on histopathology.
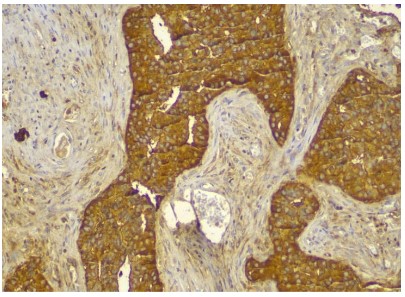
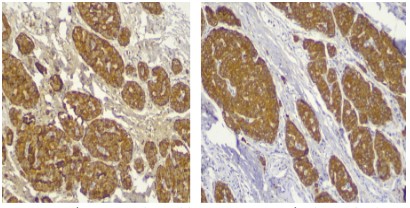
The third specimen received was omental tissue, measured 7 x 3 x 2 cms and was fibrofatty. On microscopy from multiple sections showed presence of nesting pattern with medium sized polygonal cells contain eosinophilic cytoplasm, round to oval nuclei and finely granular salt pepper chromatin. No necrosis found. Immunohistochemistry was performed.
Immunohistochemistry showed pancytokeratin positive, chromogranin positive, synaptophysin positive, CD 56 weakly positive, Leucocyte common antigen- negative with Ki-67 less than 1%. The diagnosis was suggestive of well differentiated neuroendocrine tumour.
Discussion
Cystic neoplasms of the pancreas with malignant potential are very rare, they are further classified as serous and mucinous. Majority of these tumors are benign, with only a handful of case reports of serous cyst adenocarcinomas [9-12]. These cystic epithelial lesions composed of glycogen rich cells that produce a watery fluid similar to serum. Whereas mucin-producing cystic neoplasms have a well-established malignant potential. The differentiation between benign and malignant serous cystadenoma both histologically and clinically may be very difficult. Additionally the patient admitted to our hospital with only symptoms of abdominal pain and no other specific symptoms related to varied pathologies diagnosed A thorough knowledge, experience and discussion on these rare lesion by the multidisciplinary team is very important in order to have a proper classification and treatment.
Neuroendocrine tumors are rare tumors comprising ~2% of all malignancies with the gastrointestinal tract and the lung as the most common sites. Neuroendocrine tumour express varied spectrum of proteins, shared with their normal cell counterparts at specific anatomical locations, including markers of general neuroendocrine differentiation such as chromogranin A, chromogranin B, and synaptophysin along with site-specific markers such as hormones and transcription factors [13]. In our case we found omental deposits for neuroendocrine tumour we had thought process as these might came from pancreas so performed extensive sampling but no neuroendocrine tumour found in pancreas and the findings in omental tissue along with immunohistochemistry were suggestive of neuroendocrine tumour.
Our case become exceptionally rare after diagnosis of the third all together different pathology as tuberculosis of spleen. The patient neither had a history of tuberculosis nor showed any indication of tuberculosis in the other organs by imaging studies. Clinical and routine laboratory findings were non-specific. There were no specific symptoms for establishing the diagnosis of splenic tuberculosis. In our case, the chief complaint was abdominal discomfort, without fever, anorexia or weight loss. So far, histopathological examination is still an ideal method to confirm the diagnosis. Like the treatment of pulmonary tuberculosis, antitubercular treatment is the primary modality in treating splenic tuberculosis.
The lesion was extensively studied with imaging (CT), histopathology, serology and blood tests with all these diagnostic modalities we were able to reach the diagnosis and treated the patient with magnex forte, augmentin, amikacin, pantocid, dynapar, spirometry and other supportive treatment. Patient was given antitubercular medicine with pneumococcal injection. She was discharged successfully after five days of hospital stay. Patient came for follow up and was having no complication.
Pancreatic serous cystadenocarcinoma, Splenic tuberculosis and Neuroendocrine deposits in mesentric fat such an astonishing finding of Tri pathology in a young female in three different tissue. We reviewed the slides with extensive sampling but there was no neuroendocrine component present in pancreas and no foci of any adenocarcinoma was seen in spleen and mesentry.
The case was discussed with multidiciplinary team and decided the patient to come for follow up after a month. The treatment given was antibiotics and antitubercular drugs. After a month patient came for follow up and she was absolutely normal and gave us the consent to publish her case.
As the incidental findings of tubercular spleen and neuroendocrine deposits in omental tissue was seen in our patient, we extensively search literature on pubmed and medline and did not find any such kind of case report till date. Our case might be the first case in the world with different pathologies in a same patient who is younger with age of twenty-eight years, along with it literature search showed that serous cystadenocarcinoma is present in elderly patient while our patient was young. Thus our case described exceptionally rare presentation of multiple diseases in same patient.
Declarations
Consent: Written informed consent was taken from the patient for publication of this case report along with images.
Conflict of interest: Nil.
References
- Kishida Y, Matsubayashi H, Okamura Y, Uesaka K, Sasaki K, et al. A case of solid-type serous cystadenoma mimicking neuroendocrine tumor of the pancreas. Journal of Digestive Diseases. 2014; 15: 211-215.
- Machado MC, Machado MA. Solid serous adenoma of the pancreas: an uncommon but important entity. European Journal of Surgical Oncology. 2008; 34: 730-733.
- Compagno J, Oertel JE. Microcystic adenomas of the pancreas(g lycogenrichcystadenomas). Am J ClinPathol. 1978; 69: 289-298.
- Capella CSE, Klöppel G, Hruban RH. Serous cystic neoplasms of the pancreas, in Pathology and Genetics of Tumours of the Digestive System. WHO Classification of Tumors., A.L. Hamilton SR, Editor 2000; IARC Press: Lyon. 231-233.
- Compagno J, Oertel JE. Mucinous cystic neoplasms of the pancreas withovert and latent malignancy (cystadenocarcinoma and cystadenoma): Aclinicopathological study of 41 cases. Am J ClinParhol. 1978; 69: 573-558.
- Solcia E, Kloppel G, Sobin LH 2000 Histological typing of endocrine tumours. 2nd ed. Heidelberg: World Health Organization.
- Rindi G, Villanacci V, Ubiali A. Biological and molecular aspects of gastroenteropancreatic neuroendocrine tumors. Digestion. 2000; 62: 19-26.
- Singh B, Ramdial PK, Royeppen E, Moodley J, Chetty R. Isolated splenic tuberculosis. Trop Doct. 2005; 35: 48-49.
- Yoshimi N, Sugie S, Tanaka T, Aijin W, Bunai Y, et al. A rare case of serous cystadenocarcinoma of the pancreas. Cancer. 1992; 69: 2449-2453.
- Strobel O, Z’Graggen K, Schmitz-Winnenthal FH, Friess H, Kappeler A, et al. Risk of malignancy in serous cystic neoplasms of the pancreas. Digestion. 2003; 68: 24-33.
- Siech M, Tripp K, Schmidt-Rohlfing B, Mattfeldt T, Widmaier U, et al. Cystic tumours of the pancreas: diagnostic accuracy, pathologic observations and surgical consequences. Langenbecks Arch Surg.1998; 383: 56-61.
- Horvath KD, Chabot JA. An aggressive resectional approach to cystic neoplasms of the pancreas. Am J Surg. 1999; 178: 269-274.
- Inzani F, Petrone G, Fadda G, Rindi G. Cyto-histology in NET: what is necessary today and what is the future? Rev Endocr Metab Disord. 2017; 18: 381-391.