Japanese Journal of Gastroenterology Research
Short Report - Open Access, Volume 2
Mini-invasive approach for end-stage achalasia
Daniel Velasco Hernández N*; Lucas A Rivaletto; María M Zicavo; Fernanda García Vaz; Elina Abeleyra
Department of Surgery, University Hospital General San Martín of La Plata city. Buenos Aires, Argentina.
*Corresponding Author : N Daniel Velasco Hernández
Department of Surgery, University Hospital General San
Martín of La Plata city. Buenos Aires, Argentina.
Email: daniels84@hotmail.com
Received : Nov 07, 2022
Accepted : Dec 09, 2022
Published : Nov 16, 2022
Archived : www.jjgastro.com
Copyright : © Velasco Hernández ND (2022).
Citation: Velasco Hernández ND, Rivaletto LA, Zicavo MM, Vaz FG, Abeleyra E. Mini-invasive approach for end-stage achalasia. Japanese J Gastroenterol Res. 2022; 2(16): 1124.
Introduction
End-stage achalasia is characterized by a significant esophageal dilatation added to the presence of tortuosity with a clinical presentation of progressive malnutrition and, in general, with a failure in the traditional surgical myotomy [1,2]. The objective is to present a group of patients treated with megaesophagus due to end-stage achalasia.
Material and methods
In the period between March 2008 and December 2021, 7 patients were treated minimally invasively for presenting mega esophagus due to achalasia at the end of stage (Figure 1).
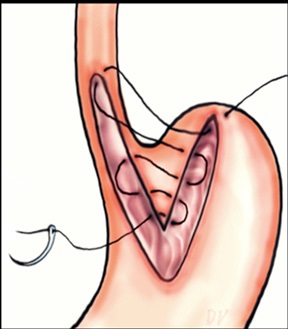
Of the total, 3 corresponded to the male sex and 4 to the female sex. The average age was 54.7 with a range of 35 to 66 years. One case corresponded to a megaesophagus of Chagasic origin, and the other 6 cases were due to recurrence of the Heller-Dor myotomy, which was treated with endoscopic dilations. The treatments performed were: 1 laparoscopic transhiatal esophagectomy and a minimally invasive esophagectomy in the prone position (Figure 2) 4 esophagus ardioplasty procedures, as described in Figure 3, and 1 case of resection of the esophagogastric junction and Roux-en-Y bypass.
Results
As postoperative complications, a case of pneumonia was recorded in the patient who underwent transhiatal esophagectomy. In cases where esophagus cardioplasty was performed, gastroesophageal reflux was notorious, but with significant relief of dysphagia and adequate weight recovery. The patient with Roux-en-Y bypass had a fistula as a complication that required reoperations for lavage and drainage. There was a loss of follow-up in the patient who underwent transhiatal esophagectomy and in another who underwent esophagus cardioplasty, the other patient who received this same treatment died at three years due to his chagasic cardiomyopathy. The other two patients continue with periodic controls.
Discussion
In the management of the final stage of achalasia, the strategy must be focused on the preservation of the organ. Recurring symptoms after surgical myotomy should be managed with endoscopic myotomy (POEM), re-Heller, or on-demand pneumatic dilations [1-4]. Before resection of the esophagus, there are some procedures such as esophagus cardioplasty, as presented in our series, which is a valid alternative to improve dysphagia, although it is highly questioned due to the significant reflux that it entails [5]. Recently in a publication by Ithurralde et al. an option is described that consists of esophageal transection and reconstruction through an intestinal loop with “Rouxen-Y” anastomosis; it seems to have very satisfactory results, so it could be considered an alternative treatment before esophagectomy [5]. Despite all these conservative therapeutic options, patients must be followed up rigorously to detect the need for an esophagectomy early. One of its predictive factors is massive dilatation of the organ (diameter greater than 6 cm) [7,8]. Therefore, esophagectomy continues to be a potential indication in patients with recurrent achalasia and radiological progression of the disease in the event of failure. of all minimally invasive treatments.
References
- Devaney EJ, Lannettoni MD, Orringer MB, Marshall B. Esophagectomy for achalasia: Patient selection and clinical experience. Ann Thorac Surg. 2001; 72: 854-858.
- Glatz SM, Richardson JD. Esophagectomy for end stage achalasia. J Gastrointestinal Surg. 2007; 11: 1134-1137.
- Ewen A Griffiths, Peter G Devitt, Glyn G Jamieson, Jennifer C Myers, Sarah K Thompson. Laparoscopic stapled cardioplasty for end-stage acalasia. J Gastrointest Surg. 2013; 17: 997-1001.
- Menezes MA, Andolfi C, Herbella FA, Patti MG. Highresolution manometry findings in patients with achalasia and massive dilated megaesophagus. Dis Esophagus. 2017; 30: 1-4.
- Aquino JL, et al. Esophagocardioplasty as surgical treatment in relapsed non advanced megaesophagus. Arq Bras Cir Dig. 2012; 25: 20-24.
- Ithurralde Argerich J, Cuenca-Abente F, Faerberg A, Rosner L, Duque-Seguro C, et al. Resection of the gastroesophageal junction and Roux-en-Y reconstruction as a new alternative for the treatment of recurrent achalasia: Outcomes in a short series of patients. J Laparoendosc Adv Surg Tech. 2019.
- Zaninotto G, Bennet C. The 2018 ISDE achalasia guidelines. Diseases of the Esophagus. 2018; 1-29.
- Loviscewk MF, Wright AS, Hinojosa WM, Petersen R, Pajitnov D, et al. Recurrent dysphagia after Heller myotomy: is esophagectomy always the answer? J Am Coll Surg. 2013; 216: 736-743.