Japanese Journal of Gastroenterology Research
Research Article - Open Access, Volume 2
Seroprevalence of Hepatitis B virus in multitransfused beta-thalassemic patients in Pakistan
Muhammad Saad Uppal1; Rehan Uppal1; Aftab Ahmad Khan1; Zahra Zahid Piracha2; Umar Saeed1,2*
1Department of Research and Development, Islamabad Diagnostic Center (IDC), F8 Markaz Islamabad (44000), Pakistan.
2International Center of Medical Sciences Research, Islamabad (44000), Pakistan.
*Corresponding Author : Umar Saeed
Department of Research and Development, Islamabad Diagnostic Center (IDC), F8 Markaz Islamabad
(44000), Pakistan.
Email: umarsaeed15@yahoo.com
Received : oct 13, 2022
Accepted : Nov 04, 2022
Published : Nov 09, 2022
Archived : www.jjgastro.com
Copyright : © Saeed U (2022).
Abstract
Background: Hepatitis B virus (HBV) is a major health problem worldwide with 2 billion people living with this virus around the globe. The major transmission route of this virus is blood and blood products. Thalaseemic patients received blood transfusions throughout their life and are at high risk of getting blood borne pathogens like HBV.
Objectives: The aim of the study is to evaluate the prevalence of Hepatitis B virus and different transfusion related parameters in Thalaseemic patients in Pakistan.
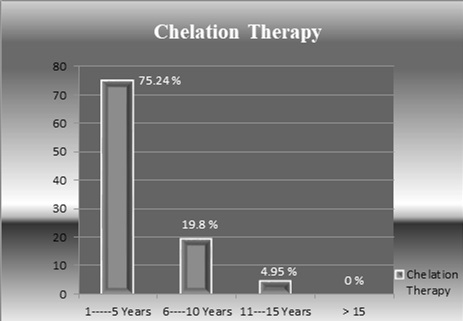
Patients and methods: A cross sectional study was conducted from January 2021 to August 2022 from Pakistan and 500 thalaseemic patients were enrolled in this study. The presence of Hepatitis B virus, hepatomegaly, splenomegaly, splenectomy, pre-transfusion haemoglobin count, Alanine Amine Transferase (ALT) level, serum creatinine, age at diagnosis of β-thalassemia, number of blood transfusions per month and therapy used were studies in this project.
Results: The prevalence of HBV is 3.08% in thalaseemic patients. Hepatomegaly was observed in 74.8% of individuals with average increase of 4.17 cm in liver size. Splenomegaly was observed in 64.9% of patients while splenectomy was observed in 14.5% of patients. The average hemoglobin count prior to blood transfusion was 8.8 g/dl. The average serum ALT was observed 92.62 U/L while the average serum creatinine was observed 0.37 mg/dl. The average age at the diagnosis of β-thalassemia was 7.7 months and the average age at first blood transfusion was 10 months. 60.68% of β-thalassemia patients had family history of this disease and average rate of transfusions was 25 blood transfusions per year. 38.55% of thalaseemic patients received chelation therapy and used desferoxamine as therapeutic option.
Conclusion: The prevalence of HBV is in intermediate zone in Pakistani population. The trend of increase in prevalence of HBV with increase in patient age is observed. Most of thalaseemic patients have family history of disease. Splenomegaly and hepatomegaly is directly proportional to the number of blood transfusions.
Keywords: Hepatitis B virus; Thalassemia; Blood transfusions; Prevalence; Hepatomegaly.
Citation: Uppal MS, Uppal R, Khan AA, Piracha ZZ, Saeed U. Seroprevalence of Hepatitis B virus in multitransfused betathalassemic patients in Pakistan. Japanese J Gastroenterol Res. 2022; 2(14): 1118.
Introduction
Hepatitis B Virus (HBV) infection is one of the most prevalent global public health problem. About 2 billion people are living with HBV worldwide out of which 400 million have chronic HBV infection [1-4]. Approximately one-third to two-third of chronically infected patients are unaware of their illness [5]. Asymptomatic spread of chronic infection is major dilemma, which significantly contributes toward dissemination of lethal viral infection to others in society [6]. It is estimated that one-third of world`s population has serological evidence of HBV infection [7]. Among chronically infected HBV patients, 15-25% develop HBV related liver cancer and cirrhosis [8]. HBV is considered as 10th leading cause of mortality in world [9,10]. The Centre for Disease Control and Prevention, USA (2008) estimated Hepatitis B Virus to be 10 and 100 times more infectious than Hepatitis C Virus and Human Immunodeficiency Virus respectively. Although HIV is considered as more contagious virus, yet worldwide prevalence of HBV is 10 times greater than HIV infection. Worldwide, on average, the HBV infection causes death of one patient every 30-45 seconds. Both HBV and HCV infection constitutes 530 million of the 6 billion world population [11,12]. Hepatitis B virus related end stage liver disease is responsible for one million deaths annually. A population with prevalence of HBV with a carrier rate of 8% or more would represent a high prevalence area; whereas population with carrier rate of 2%-7% positivity of HBV would be termed as intermediate prevalent area [8].
Pakistan stands in the HBV zone of intermediate prevalent area with 3-4% carrier rate [14-16]. HBV infection is endemic in Pakistan. It is estimated that 9 million people are HBV infected and its infection rate is increasing day by day [17,18]. It is a well-known fact that HBV can be transmitted via horizontal transmission route as well as by vertical transmission route [1,19]. The horizontal transmission in early childhood is major contributing factor for chronic viral hepatitis infection in Pakistan [20]. The perinatal transmission is leading cause of high rate of chronic infection in developing countries of Asia and Africa, whereas parenteral transmission is frequent cause of cases reported from developed industrialized countries [21]. Pakistan is a developing country of 187 million people with higher burden of infectious diseases [22]. Human development index of United Nations has ranked it 145th out of 187 countries [23]. Genetic and congenital diseases are the major causes of early death and chronic disability. In Pakistan, thalassemia is presumed to be the most common fatal genetic disorder. For any marriage between two homozygous thalassemia carriers, the probability of giving birth to child, suffering from thalassaemia minor and major, would be 50% and 25% respectively; while 25% are likely to have healthy pregnancy [24,25].
USA: Central Intelligence Agency 2007 reported world`s largest fertility rate in Pakistan, i.e. exceeding 4 children per woman [26]. The proportion of marrying to cousins and relatives is higher in Pakistan as compared to other North African Muslim countries [27]. It has been reported that 82.5% of the parents of thalassemia children had cousin marriages, with extended family history of thalassemia positive cases. 87.5% of them were unaware of risk of genetically inherited disorders and their association with consanguinity [28]. Low educational standards, poor health status and non-implementation of international blood transfusion standards are the major cause of developing Transfusion Transmitted Infections (TTIs) including HBV, HCV and HIV. Although there exist an increased threat of viral infection among high risk multitransfused population, yet due to limited resources and awareness; only a few studies have been reported from Pakistan. This article describes seroprevalence of Hepatitis B virus in multitransfused thalassemia patients in Pakistan. Relationships among HBV positivity and multiple study variables were contemplated and statistically evaluated. Current study proposes importance of non-fragmented, organized and non-hospital based, nationally centralized hygienic blood transfusion setups. It also provides valuable justifications for implementation of blood safety laws in various public health sectors of Pakistan.
Materials and methods
A cross sectional study was conducted during the period of January 2021 to August 2022 among β-thalassaemia patients with multiple blood transfusion history. 1500 thalassaemia patients were enrolled, on the basis of random sampling technique. The study was approved by institutional ethical review committee. Among all participants, β-thalassemia type-major was considered for contemplation, whereas patients having β-thalassemia type-minor and alpha-thalassemia type minor/major were excluded. Patients having previous history of repeated blood transfusions (in the form of blood cells instead of whole blood) were included for further analysis. Non responding patients with severe health complications were excluded from study. Complete physical and clinical examination was conducted for each subject. Informed written consent and patient history data was acquired from all participants. All patients were interviewed for demographic data and information regarding age at diagnosis of β-thalassemia type major, age at first blood transfusion, history of β-thalassemia in family, number of blood transfusions per month, type of transfusion acquired, blood group, chelation therapy and use of desferoxamine. Patients were clinically examined for hepatomegaly and splenomegaly and splenectomy via assistance of ultrasound technique. Among all participants pre-transfusion hemoglobin count, alanine transferase (ALT) count and serum creatinine level were calculated by the assistance of spectrophotometer in accordance to standard operating procedures. Sterile syringes were used to collect venous blood from patients. Blood was kept in vacutainer (EDTA) tubes containing EDTAK2 or EDTAK3 as anticoagulant.
All the subjects were screened for hepatitis B surface antigen (HBsAg) in serum via chromatographic immunoassay in accordance to manufacture instructions (Accurate Diagnostics USA) and HBV qualitative PCR analysis. The test device was significantly reliable due to 98% correlation with leading commercial HBsAg EIA test kit. The relative sensitivity, specificity and accuracy for HBV screening via this method was >99%, 96.7% and 98.3% respectively. The presence of viral DNA was confirmed by using HBV qualitative PCR analysis.
Statistical analysis was conducted on clinical dependent and independent variables by the assistance of Statistical Package for Social Sciences (SPSS) software version 17. χ² test were applied to identify relationships between HBV positivity and variables. Significance value was evaluated at 0.05 levels with 95% confidence level.
Results
Prevalence of HBV in thalassemia patients
Among 500 beta-thalassemia patients, HBV prevalence rate was 3.05%. 59.92% patients were male and 40.08% were female. Among male participants, 5 were found positive for HBV with prevalence of 3.184%; while among female participants, 3 were found HBV positive with prevalence rate of 2.85%.
Prevalence of HBV in different age groups
Among all participants, 62.21% (including 59.5% males and 40.5% females) belonged to 1-10 years of age and 2.45% of them were HBV positive. 36.26% of the total participants (including 63.16% males and 36.84% females) belonged to 11-20 years of age and 4.21% of them were HBV positive. 1.53% of the total participants (100% females) belonged to more than 20 years of age and HBV was not detected among those participants.
Family history of patients, age of thalassemia diagnosis and age at first blood transfusion
Among all β-thalassemia patients, 60.68% had extended family history of thalassemia. The average ages of diagnosis of beta-thalassemia disease and first blood transfusion were approximately 7.7 months and 10 months of age respectively.
Number of blood transfusions per month
The average rate of transfusions per month was 2.08 (25 blood transfusions per year) in all β-thalassemia patients. 38.17% of patients received 2 blood transfusions per month, 18.7% received 1 transfusion per month, 16.4% received 2.5 transfusions per month, 12.6% received 3 transfusions per month 8.4% received 1.5 transfusions per month, 3.05% received 3.5 transfusions per month and 2.68% received four blood transfusions per month.
Hemoglobin count prior to blood transfusions in thalassemia patients
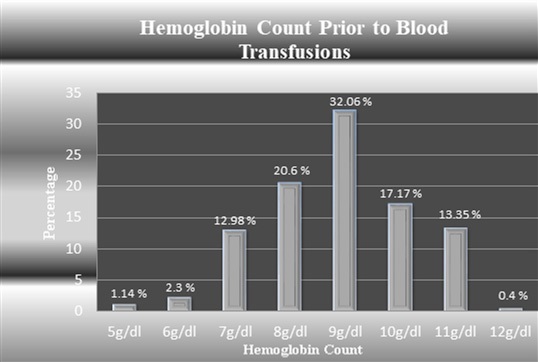
The normal range for hemoglobin count is 13.5-17.5 g/dl for males and 12-15 g/dl for females. Among all beta-thalassemia patients, the average hemoglobin count prior to blood transfusion was observed as 8.8 g/dl which significantly depicted shortage of hemoglobin count. The hemoglobin count of the participants is shown in the figure 1.
Hepatomegaly in Thalassemia patients
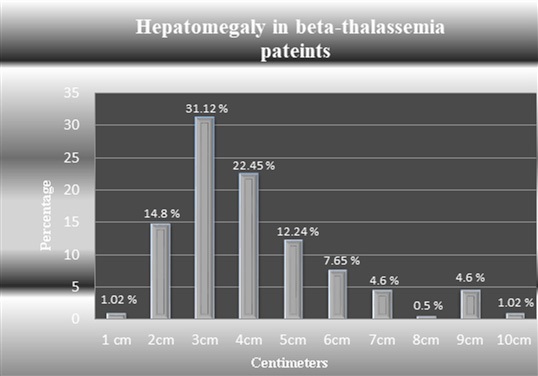
Among all beta-thalassemia patients, increase in liver size (Hepatomegaly) was observed in 74.8% individuals with average increase in liver size of approximately 4.17 cm. Majority of patients (31.12%) had 3 cm increase in liver size. Maximum increase in liver size was observed 10 cm. The hepatomegaly in thalassemic patients is summarized in figure 2.
Occurrence of normal liver and hepatomegaly with respect to age
Only 25.2% of all subjects had normal liver. 80.3% of patients with youngest age group (1-10 years of age) had normal liver while among patients of 11-20 years of age, 19.7% possessed normal liver and no case of normal liver was observed in group of participants having age more than 20 years. On average maximum increase in liver size was observed 5 cm in patients of 11-20 years of age followed by 4.25 cm in patients of more than 20 years of age while on average minimum increased liver size was observed 3.63 cm in patients of 1-10 years of age.
Hepatomegaly in Hepatitis B virus infected thalassemia patients
Hepatomegaly was observed in all the HBV positive participants. On average, 6 cm increase in liver size was observed in HBV infected patients. Most of the HBV infected thalassemia patients (37.5%) had 9 cm increase in liver size. Among HBV infected thalassemia patients, maximum increase in liver size was observed 10 cm. While rest of 62.5% of HBV infected individuals had averaged 2 cm, 3 cm, 4 cm, 5 cm and 7 cm increase in liver size with percentage occurrence of 12.5% for each category.
Relation of increase in number of blood transfusions with increase in liver size
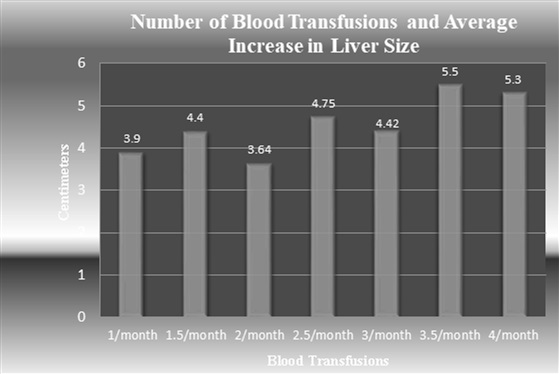
Increase in liver size was observed with respect to increased number of blood transfusions among beta-thalassemia patients. Maximum increase in liver size (5.5 cm and 5.3 cm) was observed when the 3.5 and 4 blood transfusions per month were provided to patients. An overall increasing trend (in liver size) was observed as the numbers of blood transfusions increased. The number of blood transfusions and average increase in liver size is shown in figure 3.
Splenomegaly in thalassemia patients
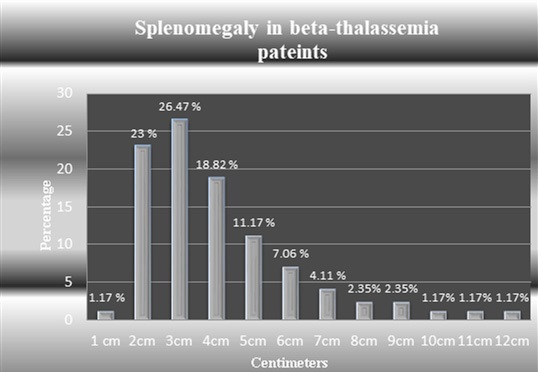
Among all thalassemia patients, splenomegaly was found among 64.9% subjects. Splenectomy was observed among 14.50% subjects with serious health complications. Among all thalassemia patients, most of the patients had 3 cm increase in spleen size; while averaged increased spleen size was 4 cm. The maximum increase in spleen size was observed up to 12 cm. Normal spleen was found only in 20.61% subjects, out of whom 70.37% belonged to age group of 1-10 years, 27.78% belonged to 11-20 years of age while only 1.85% belonged to age group of individuals having more than 20 years of age. The figure 4 represents average increase in spleen size in beta thalassemia patients.
Splenomegaly in Hepatitis B virus infected thalassemia patients
Among HBV infected beta thalassemia patients no individual had normal spleen. Splenomegaly was observed in 75% of cases while splenectomy was observed in 25% of cases. Among all HBV infected patients, most of the patients had 4cm increase in spleen size; while on average increase in spleen size was 3.16 cm.
Splenomegaly in Hepatitis B virus infected thalassemia patients
Among HBV infected beta thalassemia patients no individual had normal spleen. Splenomegaly was observed in 75% of cases while splenectomy was observed in 25% of cases. Among all HBV infected patients, most of the patients had 4cm increase in spleen size; while on average increase in spleen size was 3.16 cm.
Number of blood transfusions and increase in spleen size
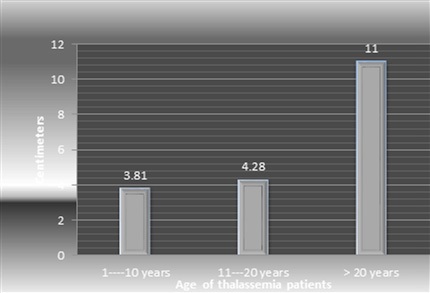
Among beta-thalassemia patients, as the number of blood transfusions were increased, an increase in spleen size was observed. Among patients who received 1 to 3 blood transfusions per month, on average, approximately 4 cm increase in spleen size was observed; while among patients who received more than 3 blood transfusions per month, on average, 5.42 cm increase in spleen size was observed. Among beta-thalassemia patients, the average maximum 11 cm increase in spleen size was observed; while among patients of 1-10 years of age the average, minimum spleen size increased was observed 3.81cm.
Occurrence of splenomegaly and splenectomy with respect to age
Among all participants, averaged maximum increase in spleen size was observed among patients of more than 20 years of age as compared to patients of 1-10 and 11-20 years of age. Figure 5 shows that the significant increase in spleen size was observed with increase in the age of beta thalassemia patients.
Splenomegaly in Hepatitis B virus infected thalassemia patients
Among HBV infected beta thalassemia patients no individual had normal spleen. Splenomegaly was observed in 75% of cases while splenectomy was observed in 25% of cases. Among all HBV infected patients, most of the patients had 4cm increase in spleen size; while on average increase in spleen size was 3.16 cm.
Number of blood transfusions and increase in spleen size
Among beta-thalassemia patients, as the number of blood transfusions were increased, an increase in spleen size was observed. Among patients who received 1 to 3 blood transfusions per month, on average, approximately 4 cm increase in spleen size was observed; while among patients who received more than 3 blood transfusions per month, on average, 5.42 cm increase in spleen size was observed. Among beta-thalassemia patients, the average maximum 11 cm increase in spleen size was observed; while among patients of 1-10 years of age the average, minimum spleen size increased was observed 3.81cm.
Occurrence of splenomegaly and splenectomy with respect to age
Among all participants, averaged maximum increase in spleen size was observed among patients of more than 20 years of age as compared to patients of 1-10 and 11-20 years of age. Figure 5 shows that the significant increase in spleen size was observed with increase in the age of beta thalassemia patients.
Statistical analysis
Mean, Median, Mode Std. Deviation, Skewness and Kurtosis observed for study variables including, age, age of diagnosis, family history of thalassemia, age at first transfusion, transfusions per month, Hb prior to transfusion, Blood amount received, Liver Size, Spleen Size, ALT and Creatinine; are shown in table 1. Various study relationships among study variables are shown in table 2. For p value less than 0.05, the relationship is considered highly significant. Among all study relationships, most were found highly significant. There also exists relationship among variables which is not highly significant as the pvalue is slightly higher than 0.05. But it does not describe absence of relationship; instead it represents comparatively less significant relationships among study variables.
Table 1: Statistical Analysis in term of Mean, Median, Mode, Std. Deviation, Skewness and Kurtosis.
Minimum |
1 |
2 |
1 |
2 |
1 |
Maximum |
28 |
48 |
2 |
168 |
4 |
Mean |
9.26 |
7.68 |
1.39 |
9.98 |
2.084 |
Median |
8 |
5 |
1 |
6 |
2 |
Mode |
4 |
3 |
1 |
3 |
2 |
Std. Deviation |
5.185 |
8.033 |
0.489 |
15.718 |
0.7445 |
Skewness |
0.714 |
3.339 |
0.44 |
5.8 |
0.334 |
Std. Error of Skewness |
0.15 |
0.15 |
0.15 |
0.15 |
0.15 |
Kurtosis |
0.4 |
-1.82 |
-1.82 |
45.2 |
-1.85 |
Std. Error of Kurtosis |
0.3 |
0.3 |
0.3 |
0.3 |
0.3 |
Statistical Analysis for Relationship Studies between Different Study Variables
Statistical Analysis |
Hb prior to transfusion |
Blood amount received |
Liver Size |
Spleen Size |
ALT |
Creatinine |
Minimum |
5 |
100 |
1 |
0 |
12 |
0.2 |
Maximum |
12 |
660 |
10 |
14 |
379 |
0.6 |
Mean |
8.87 |
263.87 |
3.374 |
2.805 |
86.42 |
0.379 |
Median |
9 |
265 |
3 |
2 |
69 |
0.4 |
Mode |
9 |
360 |
1 |
1 |
76 |
0.3 |
Std. Deviation |
1.35 |
90 |
2.1 |
2.52 |
64.7 |
0.0882 |
Skewness |
-0.216 |
0.817 |
0.928 |
1.471 |
1.904 |
0.787 |
Std. Error of Skewness |
0.15 |
0.15 |
0.15 |
0.15 |
0.151 |
0.15 |
Kurtosis |
-0.252 |
2.608 |
0.687 |
2.7 |
4.417 |
-0.225 |
Std. Error of Kurtosis |
0.3 |
0.3 |
0.3 |
0.3 |
0.3 |
0.3 |
Table 2: Statistical Analysis for Relationship Studies among different study variables.
Relationship Between Variables |
Pearson Chi-Square |
P-value |
test value |
(Confidence level) |
|
Relationship Between Age of Diagnosis and Age at First Blood Transfusion |
2.37 E 3 |
0 |
Relationship Between Number of Blood Transfusions and Increase in Liver Size |
2.53 E 2 |
0 |
Relationship Between Number of Blood Transfusions and Increase in Spleen Size |
2.29 E 2 |
0 |
Relationship Between Hepatomegaly with Age |
6.21 E 2 |
0 |
Relationship Between Hepatomegaly and HBV Positive Thalassemia Patients |
34.443 |
0.002 |
Relationship Between Splenomegaly with Age |
7.419 E 2 |
0 |
Relationship Between Splenomegaly with HBV Positive Thalassemia Patients |
14.487 |
0.755 |
Relationship Between Age and Amount of Blood Received |
1.541 |
0 |
Relationship Between Age and ALT Level |
3.68 E 3 |
0 |
Relationship Between Age and Creatinine Level |
1.372 E 2 |
0.001 |
Relationship Between HBV Positive Individuals and ALT Level |
2.10 E 2 |
0 |
Relationship Between HBV Positive Individuals and Creatinine Level |
5.406 |
0.248 |
Discussion
Beta-thalassemia is autosomal recessive disorder widely distributed around world including China, Indonesia, Maley, Peninsula, Middle East, Burma, Africa, Southeast Asia and Indian subcontinent. Among different regions of world, its estimated rate of gene frequency is 3% to 10% [29]. Thalassemia is being considered as one of the most threatening global health problem for upcoming 50 years with major burden on world`s blood bank supplies. The carrier rate of this disease varies depending upon different areas of world. The carrier rate of thalassemia in Indian subcontinent and China, Central Asia, North Mediterranean and Arab region is approximately 1-40%, 4-10%, 1-19% and 3% respectively. The prevalence of thalassemia is highest in Eastern Mediterranean Region (EMR) as compared to other parts of world [30].
In Pakistan, the annual number of infants born with beta thalassemia is significantly higher as compared to other EMR regions. It has been reported that 5,000-9,000 children are born with β-thalassaemia per year in Pakistan. The approximate carrier rate is 5% to 7% with 9.8 million carriers [31]. Some of the possible preventive measures to reduce thalassemia in Pakistan includes; extended family screening for thalassemia, genetic counseling of couples at risk, prenatal diagnosis of thalassemia and termination of pregnancy (before fetal age of 19 weeks/120 days) [32]. The consanguineous and tribal marriages are frequent in both rural and urban areas of Pakistan due to limited awareness, negative role of culture, negative behavior of general public and poor genetic counseling. There exist a strong relation between consanguineous marriages and thalassemia. The premarital screening, cultural, ethnic, religious and social issues must be resolved. Informed consent and guarantees of privacy are also important parameters for the success of premarital screening programs.
The seroprevalence of HBV infection varies in different parts of world, it has been reported that HBV is prevalent up to 5% in India, while in Italy, Russia and Turkey the prevalence rate ranges from 3%-10% [33-36]. In Pakistan, approximately 7 to 9 million people are living with HBV having approximate carrier rate of 3% to 5% [1]. There exist significant differences in prevalence of hepatitis B virus among various populations. In general population, the prevalence of HBV was reported as 4.5% and 2.3% [17,37]. The prevalence of HBV in peds was reported as 1.8% [9]. Prevalence of HBV in pregnant women significantly varies between ranges of 0.34% to 12.62% in different regions of Pakistan, depending upon environment and hygiene [38,39]. Several seroprevalence studies have been conducted on blood transfusion populations from Peshawar, Rawalpindi, Abottabad, Multan, Bahawalpur, Quetta and Karachi; with HBV prevalence rate of 2.51%, 1.9%, 3.3%, 1.55%, 4.93%, 2.69%, 4.80% and 4.90% respectively [40-44,14, 45,46].
According to Farooqi et al, the prevalence of HBV in thalassemia patients was 2.28% [6] while our study shows the prevalence of 3.05%. Our study has identified prevalence of HBV and associated important study variables including Age, Sex, Age at Diagnosis of β-thalassemia Type Major, History of β-Thalassemia in Family, Age at First Blood Transfusion, Number of Blood Transfusions per Month, Pre-transfusion Hemoglobin Count, Quantity of Blood Provided, Hepatomegaly, Splenomegaly, Splenectomy, Alanine transferase (ALT) Count, Serum Creatinine Level, Type of Transfusion Acquired (Whole Blood/ Blood Cells), Type of Thalassemia (Minor/ Major), Type of blood group, Chelation Therapy and Use of Desferoxamine. Up to date no scientific study has been conducted from Pakistan depicting valuable information regarding aforementioned study variables and their association with HBV.
Hepatitis B was found more prevalent in male participants as compared to females. Young beta thalassemia patients were comparatively less HBV infected as compared to elder beta thalassemia patients, possibly due to less exposure to risky blood transfusions. Majority of participants had extended family history of thalassemia. According to Shah et al from India, among young patients of 0-5 years of age, majority of blood transfusions were offered once per month but when the age of patients increased up to 20-25 years, the numbers of blood transfusions were also increased up to four times per month depending upon patient’s health [47]. Our study has also identified similar trend among beta thalassemia patients of different age groups.
Majority of study participants had significant shortage of hemoglobin count prior to blood transfusions. Only 0.40% of the participants had hemoglobin within normal range. Least observed hemoglobin count among patients with serious health complications was 5 g/dl. Poor patients with inadequate food and health facilities depicted significantly lower level of hemoglobin count. Unfortunately the blood transfusion setups are disorganized in rural areas and more than sixty percent of Pakistani nation belongs to rural areas with poor health facilities. In order to seek medical treatment, villagers travel large distances to developed cities. In such circumstances, due to lack of money, most of innocent villagers find cheap medical treatment options. In most of the cases, when there is an increased demand for blood, the poor individuals switch towards replacement or paid blood donations. In-appropriate screening of blood prior to blood transfusions, can bring havoc in their lives.
In thalassemia patients, the liver problems are generally caused due to iron overload or viral infection or both. In present study we found that 75% of participants had abnormally enlarged liver with maximum increase up to 10 cm. While in HBV positive individuals, hepatomegaly was observed with 100% rate. It is reported from Bangladesh that 100%, 99%, 7.5% and 3.5% of thalassemic patients had hepatomegaly, splenomegaly, oedema and clubbing respectively [48]. Our study states that among all thalassemia patients, 31.12% had 3cm increase in liver size while 37.5% of HBV positive beta thalassemia patients had 9 cm increase in liver size.
Cases with normal liver condition also existed. It was found that youngest age grouped individuals had more number of normal liver conditions as compared to older age group individuals. Among youngest group of individuals averaged increase in liver size of 3.63 cm was significantly less compared to older patients with averaged increased liver size up to 5 cm. Hussain et al reported that, on average 24 blood transfusions are required by thalassaemia patients [24]. But according to our study, on average, 25 blood transfusions are required per year for thalassemia patient. Our study has identified significantly increasing trend between relationship of increase in liver size and number of blood transfusions. It was evident that as the number of blood transfusions increased from one to four transfusions per month, significantly increase in liver size was observed.
Our study states that majority (65%) of patients had abnormally increased spleen size with maximum increase up to 12 cm. In HBV infected patients no case was observed with normal spleen, instead splenomegaly was observed in 75% of cases while rest of the individuals had splenectomy. Only few cases of normal spleen were found in youngest age grouped individuals. As the age of individuals increased, chances of occurrence of normal spleen decreased. Majority of beta thalassemia patients (26.47%) had 3 cm increase in spleen size but in HBV infected beta thalassemia patients most of the patients (38%) had 4 cm increase in spleen size.
Our study has identified a relationship between number of blood transfusions and increase in spleen size. Patients who received 3 or less than 3 blood transfusions per month had approximately 4 cm averaged increase in spleen size but when transfusions exceeded 3 blood transfusions per month, on average, 5.42 cm increase in spleen size was observed. Our study has also identified strong relationship between age, splenomegaly and splenectomy. It is evident that the patients had more than 20 years age had significantly increase in spleen size i.e. up to 11 cm and majority of splenectomy cases (66.67%) belonged to this group. HBV infected patients had significantly higher level of ALT compared to beta-thalassemia patients in general. But the serum creatinine level was approximately same in both HBV positive and HBV negative individuals.
Identification of most appropriate donors and ensuring proper blood screening prior to donations are the key factors associated with safe blood donation. For safe blood donation, the donors must possess repeated negative results for blood borne pathogens. Blood requirements are on its peak during pregnancy related issues, traumatic injuries, thalassemia, dialysis, hemophilia. In order to cope with such emergency situations; organized, fair and safe blood transfusion setups must be developed at national level with easy accessibility. There is an urgent demand for implementation of international blood safety standards at various blood transfusion setups to ensure limited risk for transmission of hepatitis B virus.
Conclusion
From this study we conclude that HBV is frequently proliferating in multitransfused beta-thalassemic patients in Pakistan. The major reason for increased prevalence is inadequate screening facilities available for donors. Males are more HBV infected as compared to females. The HBV was more prevalent in thalassemia patients with higher age group. Hepatomegaly and Splenomegaly was present in majority of thalassemia patients. As the number of blood transfusions was increased, increase in liver and spleen size was observed. Splenectomy was also observed in hepatitis infected thalassemia patients. Most of the enrolled thalassemia patients had previous family history of thalassemia and majority of them were using desferoxamine. Our study provides solid background information for future investigators working on epidemiological patterns of HBV and HCV in high risk population (especially multitransfused thalassemia populations. Owing to dearth of adequate screening resources against transfusion transmitted infections (like HBV, HCV and HIV), strict criteria of safe donor selection should be adopted to miniaturize economic burden of diseases. Our study proposes importance of non-fragmented, organized and non-hospital based, nationally centralized hygienic blood transfusion setups. It also provides valuable justifications for implementation of blood safety laws in various public health sectors of Pakistan.
References
- Ali M, Idrees M, Ali L, Hussain A, Rehman I, et al. Hepatitis B virus in Pakistan: A systematic review of prevalence, risk factors, awareness status and genotypes. Virology Journal. 2011; 8: 102.
- Li G, Li W, Guo F, Xuc S, Zhaod N, et al. A novel real-time PCR assay for determination of viral loads in person infected with hepatitis B virus. J Virol Meth. 2010; 165: 9-14.
- Zhu R, Zhang H, Yu H, Li H, Ling YQ, et al. Hepatitis B virus mutations associated with in situ expression of hepatitis B core antigen, viral load and prognosis in chronic hepatitis B patients. Pathol Res Pract. 2008; 204: 731-742.
- Alam MM, Zaidi SZ, Malik SA, Naeem A, Shaukat S, et al. Serology based disease status of Pakistani population infected with Hepatitis B virus. BMC Infect Dis. 2007; 7: 64.
- Ward J. Improving diagnosis of chronic Hepatitis B virus; updated CDC guidelines on population recommended for testing and specific test conditions. Education webcast sponsored by Abbot diagnostic 2009.
- Farooqi JI, Farooqi RJ, Khan N, Mussarat. Frequency of hepatitis B and C in selected groups of population in NWFP, Pakistan. JPMI. 2007; 21: 165-168.
- De-Franchis R, Hadengue A, Lau G, Lavanchy D, Lok A, et al. EASL International Consensus Conference on Hepatitus B Consensus statement. J Hepatol. 2003; 39: S3-25.
- Weinbaum CM, William I, Mart EE, Wang SA, Finelli L, et al. Recommendation for identification and public health management of person with chronic HBV infection. MMWR. 2008; 8: 1-20.
- Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004; 11: 97-107.
- Waheed Y, Rahat TB, Safi SZ, Qadri, I. Epidemiological patterns and risk factors associated with hepatitis B virus in Pakistani population. Asian Biomed. 2010; 4: 547-554.
- Hwang LY, Krammer JR, Troisi C, Bull L, Grimes CZ, Lyerla R, et al. Relationship of cosmetic procedures and drug use to hepatitis C and hepatitis B virus infections in a low-risk population. Hepatology. 2006; 44: 341-351.
- World Health Organization. Hepatitis C WHO Fact sheet 164. 2000.
- National Foundation for Infectious Diseases 2012.
- Fayyaz M, Khan MA, Qazi MA, Chaudhary GMD, Ahmed G. Hepatitis B, C and HIV: sero-prevalence of infection in blood donors. Profess Med J. 2006; 13: 632-636.
- Andre F. Hepatitis B epidemiology in Asia, Middle east and Africa. Vaccine. 2000; 1: S20-22.
- Waheed Y, Saeed U, Safi SZ, Chaudhry WN, Qadri I. Awareness and risk factors associated with barbers in transmission of hepatitis B and C from Pakistani population: barber’s role in viral transmission. Asian Biomedicine. 2010; 4: 435-442.
- Noorali S, Hakim ST, McLean D, Kazmi SU, Bagasra O. Prevalence of hepatitis B virus genotype D in females in Karachi, Pakistan. J Infect Devel Count. 2008; 2: 373-378.
- Hakim ST, Kazmi SU, Bagasra O. Sero prevalence of Hepatitis B and C Genotypes Among Young Apparently Healthy Females of Karachi- Pakistan. Libyan J Med. 2008; 3: 66-70.
- Jafri W, Jafri N, Yakoob J, Islam M, Tirmizi SFA, et al. Hepatitis B and C: prevalence and risk factors associated with seropositivity among children in Karachi, Pakistan. BMC Infect Dis. 2006; 6: 101.
- Abdul-Mujeeb S, Jamal Q, Khanani, R, Iqbal N, Kaher S. Prevalence of hepatitis B surface antigen and HCV antibodies in Hepatocellular carcinoma cases in Karachi, Pakistan. Trop Doct. 1997; 27: 45-46.
- Maddrey WC. Hepatitis B: an important public health issue. J Med Virol. 2000; 61: 362-366.
- Wikipedia, Demographics of Pakistan 2010.
- Wikipedia, List of Countries by Human Development Index, 2010.
- Hussain H, Iqbal R, Khan MH, Iftikhar B, Aziz S, et al. Prevalence of hepatitis C in Beta thalassaemia major. Gomal J Med Sci. 2008; 6: 87-90.
- Lee GR, Bithell TC. Wintrobe’s Clinical Hematology beta- thalassemia.1993; 1: 1106-1117.
- World fact book. Pakistan USA: Central Intelligence Agency 2007.
- Afzal M, Ali SM, Siyal HB. Consanguineous Marriages in Pakistan. The Pakistan Development Review. 1994; 33: 663-676.
- Arif F, Fayyaz J, Hamid A. Awareness among parents of children with thalassemia major. J Pak Med Assoc. 2008; 58: 621-624.
- Weatherall DJ, Clegg JB. Thalassaemia- a global public health problem. Nat Med. 1996; 2: 847-849.
- Angastiniotisa M, Modell B. Global Epidemiology of Hemoglobin Disorders. Ann N Y Acad Sci. 1998; 850: 251-269.
- Ahmed S, Saleem M, Modell B, Petrou M. Screening extended families for genetic hemoglobin disorders in Pakistan. N Engl J Med. 2010; 347: 1162-1168.
- Iqbal I. Prevention of Thalassemia in Pakistan. Nish Med J. 2009; 1: 1-3.
- Kurien T, Thyagarajan SP, Jeyaseelan L. Community prevalence of hepatitis B infection and modes of transmission in Tamil Nadu, India. Indian J Med Res. 2005; 121: 670-675.
- Iashina TL, Favorov MO, Shakhgil’dian IV. The prevalence of the markers of viral hepatitis B and delta among the population in regions differing in the level of morbidity. Vopr Virusol. 1992; 37: 194-196.
- Erden S, Buyukozturk S, Calangu S. A study of serological markers of hepatitis B and C viruses in Istanbul, Turkey. Med Princ Pract. 2003; 12: 184-188.
- Da-Villa G, Sepe A. Immunization programme against hepatitis B virus infection in Italy: cost-effectiveness. Vaccine. 1999; 17: 1734-1738.
- Chaudhary IA, Shah SK, Majrooh MA, Alvi AA. Seroprevalence of hepatitis-B and C among patients reporting in surgical OPD at Fauji Foundation Hospital, Rawlapindi: Review of 5 year literature. Pak J Med Sci. 2007; 23: 514-517.
- Sheikh SM. Hepatitis B and C: value of universal antenatal screening. J Coll Physicians Surg Pak. 2009;1 9: 179-182.
- Yousfani S, Mumtaz F, Memon A, Memon MA, Sikandar R. Antenatal screening for hepatitis B and C virus carrier state at a university hospital. J Liaquat Uni Med Health Sci. 2006; 5: 24-27.
- Asif N, Khokhar N, Ilahi F. Seroprevalence of HBV, HCV and HIV infection among voluntary non remunerated and replacement donors in northern Pakistan. Pak J Med Sci. 2004; 20: 24-28.
- Ahmad J, Taj AS, Rahim A, Shah A, Rehman M. Frequency of hepatitis B and C in healthy blood donors of NWFP: A single centre experience. J Post Med Inst. 2004; 18: 343-352.
- Khattak MF, Salamat N, Bhatti FA, Qureshi TZ. Seroprevalence of hepatitis B, C and HIV in blood donors in northern Pakistan. J Pak Med Assoc. 2002; 52: 398-402.
- Ahmad F, Shah SH, Tariq M, Khan JA. Prevalence of hepatitis B carrier and HIV in healthy donors at Ayub teaching hospital. Pak J Med. 2000; 39: 91-92.
- Jehangir W, Ali F, Shahnawaz U, Iqbal T, Qureshi HJ. Prevalence of hepatitis B, C and HIV in blood donors of south Punjab. Esculapio.2006; 2: 6-7.
- Khan ZA, Aslam MI, Ali S. The frequency of hepatitis B and C among volunteer blood donors in Balochistan. Hep Mon. 2007; 7: 73-76.
- Mujeeb SA, Mehmood K. Prevalence of HBV, HCV and HIV infections among family blood donors. Ann Saudi Med. 1996; 16: 702-703.
- Shah N, Mishra A, Chauhan D, Vora C, Shah NR. Study on effectiveness of transfusion programe in thalassemia major patient receiving multiple blood transfusions in Western India. Asian J Transfus Sci. 2010; 4: 94-98.
- Uddin MR, Rana M, Islam MMSUI, Begum F, Salimullah ASM, et al. Seroprevalence of hepatitis c virus in thalassemic patients. J Dhaka Med Coll. 2009; 18: 115-119.