Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 2
Acute intussusception of Meckel’s Diverticulum in a 15-year-old boy: Clinical, imaging and laparoscopy aspects
Nyandwi Léonidas*; Haffreingue Aurore; Jean Baptiste Marret; Rod Julien
Pediatric Surgery Department, CHU Caen-Normandie, Avenue de la Côte-de-Nacre, 14033 Caen Cedex 9, France. University of Caen-Normandy, UFR Health, Caen, France.
*Corresponding Author : Nyandwi Léonidas
Pediatric Surgery Department, CHU Caen-Normandie,
Avenue de la Côte-de-Nacre, 14033 Caen Cedex 9,
France.
University of Caen-Normandy, UFR Health, Caen,
France.
Email: nyandwleo@yahoo.fr
Received : Oct 07, 2022
Accepted : Oct 20, 2022
Published : Oct 27, 2022
Archived : www.jjgastro.com
Copyright : © Léonidas N (2022).
Abstract
Acute intussusception on Meckel’s diverticulum (MD) is a rare cause of abdominal pain requiring emergency surgery. The aim of this study, is to provide an adequate level of clinical knowledge and diagnostic modalities as well as management of MD. We report an interesting case of a long symptomatic ileum intussusception and recidivist due to a MD. This case is a 15-year male adolescent with a history of chronic constipation who presented to the emergency room with acute and severe abdominal pain. An abdominal ultrasound and computed tomography (CT) finding a distal bowel intussusception. An urgently laparoscopic exploration was performed and subsequently converted to a mini-laparotomy, which revealed the intussuscepted MD without focal necrosis. A segmental small bowel resection with hand suture and primary anastomosis was performed. Histopathology found gastric antral mucosa. Finally, the patient had uncomplicated postoperative recovery and remained well upon routine follow-up. This case presents an interesting challenge in diagnosis and when deciding surgery. Laparoscopic exploration may help to diagnosis and surgery of acute intussusception due to MD.
Keywords: Acute ileum intussusception; Meckel’s diverticulum; Imaging, Pediatrics; Laparoscopy
Citation: Léonidas N, Aurore H, Marret JB, Julien R. Acute intussusception of Meckel’s Diverticulum in a 15-year-old boy: Clinical, imaging and laparoscopy aspects. Japanese J Gastroenterol Res. 2022; 2(14): 1116.
Introduction
Meckel’s diverticulum is common in 2% of the general population [1]. Most often Meckel’s diverticulum are asymptomatic, the discovery is rare in the neonatal period (0.3%) [2]. Symptomatic patients commonly present with gastrointestinal bleeding from small bowel ulcerations due to ectopic gastric acid secretion within the MD, diffuse abdominal pain from inflammation, or intestinal obstruction from volvulus or intussusception of the small bowel with MD as the lead point [3,4]. Although the patient’s age at presentation can yield imperative diagnostic cues, MD should nevertheless be considered in the list of differentials in patients presenting with acute small bowel obstruction regardless of age MD. Despite the means of imaging, in particular ultrasound, scanner, MRI, MD is often discovered during surgical exploration [2,5]. Laparoscopy allows diagnosis and treatment [6]. The anatomopathological examination of the surgical specimen found in the vast majority gastric heterotopia (71%), pancreatic (12%), duodenal, rarely endometrial tissue [7,8]. After surgery, the evolution is always good, rarely with complications. We present a case that presented intermittent abdominal pain with chronic constipation, the discovery of Meckel’s diverticulum was confirmed intraoperatively in the second acute intussusception at the age of 15 years.
Presentation of the case
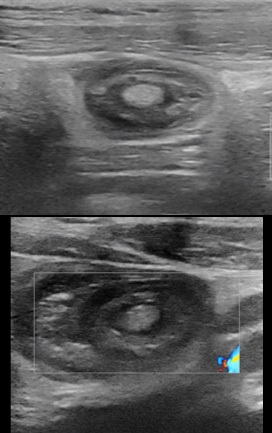
A 15-year-old male patient, with a history of intermittent abdominal pain, two episodes of bleeding considered to anal fissure, and of chronic constipation consulted twice in the emergency department for ileo-ileal intussusception more than a year apart. At the first presentation, the patient consult with the general condition preserved, apyrexia, bilious vomiting. The physical examination found pain in the right hypochondrium and sub umbilical, a soft abdomen, no tusks or palpable abdominal mass. The ultrasound performed found ileo-ileum intussusception without any sign of complication with the intussusception tube in the pelvic position (Figure1).
An hour later in the emergency room there is no more pain, a new ultrasound is requested which does not found the intussusception. He discharges and an appointment was set for him in three months in the event of no recurrence. The patient was seen again on the scheduled date and there was no recurrence or sign of complication. Seventeen months later from the first episode of invagination, the patient consults to the emergency room for episodes of severe abdominal pain localized in the epigastric region, of high intensity, without signs of irradiation and similar to those of the previous attack, no transit since two days (usual, consistent with his chronic constipation). The general condition of the patient is preserved, temperature at 36.4°C, pulse: 90 per minute, SaO2 : 100%, weight: 57.7 kg, digital pain assessment: 8, spontaneous ventilation ambient air: 18 cycles per minute, pale coloring, nauseous, but no vomiting. Physical examination revealed epigastric pain, a numb, helpless, unbloated abdomen, no palpable organomegaly. Ultrasound performed in an emergency found ileum intussusception at the epigastric location with the presence of a probable fatty structure mimiking to a mesenteric fat or a lipoma, a few visible common mesenteric lymph nodes, no coeliomesenteric or retroperitoneal adenopathy, there is no intra-abdominal fluid effusion (Figure 2).
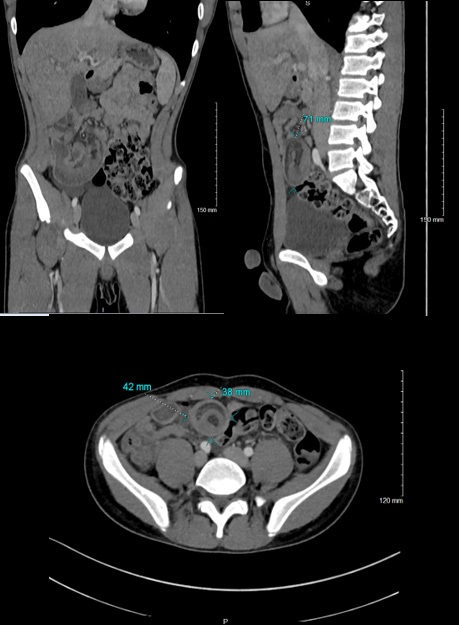
An abdominal computed tomography found the presence of an ileo-ileum intussusception in the right iliac fossa (the sausage 42 x 38 mm in diameter and 71 mm in length) whose content is a fatty image within the infiltration linked to the intussusception of the mesenteric fat, the presence of signs of early intestinal pain. Furthermore, there was no parietal enhancement defect, no identifiable underlying mass syndrome, but the presence of submillimetric nodal formations with the neighboring minor axis (Figure 3).
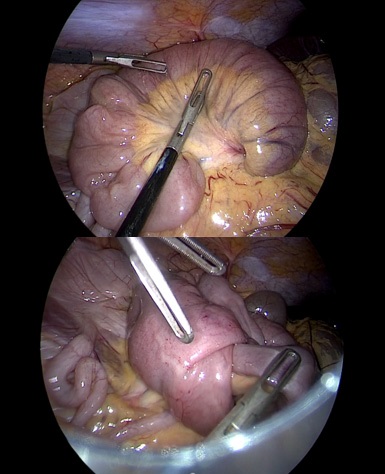
An urgently laparoscopy management found an ileo-ileum intussusception sausage in the epigastric region. The partial laparoscopic reduction of the small intestine discovers a mesenteric fat and did not complete reduction (Figure 4). A conversion to the periumbilical minilaparotomy using the Alexis retractor was done and found the MD approximately to 60 cm from the Bauhin's valve with good staining, without necrotic lesions (Figure 5). Subsequently, a segmental small-bowel resection with primary anastomosis was performed.
The surgical specimen was sent for histopathological examination for analysis. The postoperative course was simple, he recuperated gradually. On postoperative day 3, the patient was discharged from the hospital uneventfully. At follow up, he had a good improvement of the constipation, the clinical examination was normal. The results of the anatomopathological examination confirmed a MD which is contained by an ileum type mucosa with a congestive aspect, antral metaplasia without dysplasia or histological signs of malignancy. The follow up was closed because there is no need for systematic follow-up.
Discussion
Small bowel obstruction (SBO) secondary to intussusception of Meckel’s diverticulum (MD) is a rare cause of acute abdominal pain that may warrant urgent surgical treatment [9,10].
Varlik and all [11] found 3/14 case of intussusception as complication of MD. MD is often asymptomatic. The diagnosis may be challenging as the condition remains asymptomatic or may mimic various diseases and obscure the clinical picture [12]. Life-threatening complications include bleeding, obstruction by intussusception or strangulation, inflammation and perforation [4,13,14]. Our case had a long history of chronic constipation, intermittent abdominal pain, and episodes of rectal bleeding. Assumptions of anal fissures, appendicitis and gastroenteritis disorders have been issued. MD case emphasizes the importance of history and physical exam findings in coordination with radiologic imaging in helping to make appropriate decisions in a timely manner for operative vs conservative management of an SBO [15]. Bleeding is not the only presentation written about in literature, obstructive symptoms have been reported. Painless gastrointestinal (GI) bleeding is the most common presentation due to the greater predominance for ectopic gastric tissues within the MD [5,8]. Our patient did not present obstructive symptoms, but instead with GI bleeding. Different imaging studies (ultrasound, X-ray, angiography, contrast-enhanced, computed tomography, Technetium-99 scan, capsule endoscopy and magnetic resonance imaging) can be used for diagnosis but the sensitivity and specificity is low [2,16]. Radiological exams generally show complications of MD leading to surgery [14]. Qiong and all [17] developed modality of balloon-assisted enteroscopy (BAE), including double balloon enteroscopy (DBE) and single-balloon enteroscopy (SBE), was introduced, there have been some case reports in the English literature of patients with non-complicated MD which has been diagnosed by BAE. Inverted MD initially misdiagnosed in 10/74 cases by DBE and was finally confirmed by an operative procedure and pathology. In our case report, ultrasound and computed tomography found ileum intussusception secondary to the presence of a polyp or mesenteric fat. Furthermore, the diagnosis of MD as the cause for intussusception at time of operative diagnosis should be treated with a systematic thought process to first reduce the intussusception, determine viability of the tissue and treat with diverticulectomy or segmental resection [11,18,19]. Laparoscopic exploration confirms the diagnosis and the resection or combined to mini open out resection. In this report, laparoscopic exploration helps us to partially reduce ileulm intussusception, but the diverticulum invagination needed conversion to mini open surgery and then reduction, complete exploration of lesions and resection. It has been argued that reduction of an intussuscepted bowel itself may be adequate in treating intussusception as long as the tissue is viable, and it can be determined that the cause of the intussusception or lead point is benign [6]. Whether this is done clinically, by frozen or by permanent section was not discussed in literature and this is not described as the standard approach in practice. In most literature, the accepted treatment modality for an MD is diverticulectomy or segmental resection, as the risk of recurrence remains significant after reduction alone [6,11]. Gastric mucosa constitutes more than 60% of the ectopic tissue. The second common foci is pancreatic acinus, but Brunner glands, pancreas islands, colon mucosa, endometriosis and hepatobiliary tissue might also be seen [8,13]. They are many case reports, few multicentric studies or meta-analysis to determine the frequently age of of MD intussusception. All of the recent study confirm that laparoscopy exploration confrm diagnostic. Reduction of invagination maybe challenge by diverticulis strictures and need conversion to complete surgery
Conclusion
In conclusion, faced with the signs of chronic constipation, periodic abdominal pain and episodes of rectal bleeding, the diagnosis of diverticulitis by MD must be considered, and exploratory assessments remain necessary. Acute intussusception by MD is the complicated form requiring emergency surgery. Imaging, shows indirect signs. Laparoscopic remains necessary for reduction and resection.
Declarations
Consent: Written informed consent was obtained for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests: The authors declare that they have no competing interests.
References
- Choi SY, Hong SS, Park HJ, Lee HK, Shin HC, Choi GC. The many faces of Meckel’s diverticulum and its complications. Journal of Medical Imaging and Radiation Oncology. 2017; 61:225‑31.
- Sabina Giusti, Chiara Iacconi, Patrizia Giusti, Michele Minuto, Davide Caramella, Carlo Bartolozzi Ileal invaginated Meckel’s diverticulum: imaging diagnosis (2004:9b). 2004; 14: 2368‑71.
- Anwar MO, Ahmed HI, Al Hindi S, Al Omran Y. Meckel’s diverticulum with intussusception in a 5-year-old patient with Down’s syndrome. Case Reports. 2014: bcr2014207431-bcr2014207431.
- Morrison J, Jeanmonod R. Intussusception Secondary to a Meckel’s Diverticulum in an Adolescent. Case Reports in Emergency Medicine. 2011; 2011: 1‑3.
- Tazi Charki M, Oukhouya MA, Benmassaoud Z, Mahmoudi A, Khattala K, Bouabdallah Y. Complications of Meckel’s diverticulum in children: about 18 cases. Pan Afr Med J. 2019; 33.
- Zorn J, Zhang S, Brandt J, Keckeisen G. Small bowel obstruction precipitated by intussusception of Meckel’s diverticulum. SAGE Open Medical Case Reports. 2022; 10: 2050313X2110726.
- Menezes M, Tareen F, Saeed A, Khan N, Puri P. Symptomatic Meckel’s diverticulum in children: a 16-year review. Pediatr Surg Int. 2008; 24: 575‑7.
- Almas T, Alsubai AK, Ahmed D, Ullah M, Murad MF, Abdulkarim K, et al. Meckel’s diverticulum causing acute intestinal obstruction: A case report and comprehensive review of the literature. Annals of Medicine and Surgery. 2022; 78: 103734.
- Ihsan Yıldız, Yavuz Savas Koca, Ibrahim Barut. An unusual case of intraabdominal abscess and acute abdomen caused by axial torsion of a Meckel’s diverticulum. Case report. Annals of Medicine and Surgery. 2016; 6: 74e76.
- Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel’s diverticulum in the 21st century. Medicine (Baltimore). 2018; 97: e12154.
- Erol V, Yoldas T, Cin S, Caliskan C, Akgun E, Korkut M. Complicated Meckel’s diverticulum and therapeutic management. UCD. 2013; 29: 63‑6.
- Benjelloun EB, Ousadden A, Ibnmajdoub K, Mazaz K, Taleb K. Small bowel intussusception with the Meckel’s diverticulum after blunt abdominal trauma: a case report. World J Emerg Surg. 2009; 4: 18.
- Skarpas A, Siaperas P, Zoikas A, Griva E, Kyriazis I, Velimezis G, et al. Meckel’s Diverticulitis. A rare cause of small bowel obstruction. Journal of Surgical Case Reports. 2020; 2020: rjaa339.
- Luu AM, Meurer K, Herzog T, Uhl W, Tannapfel A, Braumann C. Small Bowel Obstruction due to a Giant Meckel’s Diverticulum. Visc Med. 2016; 32: 434‑6.
- Marascia DJ. Small Bowel Obstruction Secondary to Intussuscepted Meckel’s Diverticulum in an Adult. Case Reports in Surgery. 2019: 3241782.
- Kuru S, Kismet K. Meckel’s diverticulum: clinical features, diagnosis and management. Rev Esp Enferm Dig. 2018; 110: 726- 732.
- Chou JW, Chung CS, Huang TY, Tu CH, Chang CW, Chang CH, et al. Meckel’s Diverticulum Diagnosed by Balloon-Assisted Enteroscopy: A Multicenter Report from the Taiwan Association for the Study of Small Intestinal Diseases (TASSID). Gastroenterol Res Pract. 2021: 9574737.
- Evola G, Caramma S, Caruso G, Schillaci R, Reina C, Reina GA. Intestinal obstruction and ischemia by necrotic annular Meckel’s diverticulum: Case report and review of the literature. Int J Surg Case Rep. 2021; 82: 105897.
- Yu M, Fang Z, Shen J, Zhu X, Wang D, Shi Y. Double simultaneous intussusception caused by Meckel’s diverticulum and intestinal duplication in a child. J Int Med Res. 2018; 46: 3427‑34.