Japanese Journal of Gastroenterology Research
Research Article - Open Access, Volume 2
Experience of intussusception at a tertiary care hospital: A prospective study
Raghu Nandan Y*, Rajeev N
Department of General Surgery, Dr. B. R. Ambedkar Medical College and Hospital, India.
*Corresponding Author : Raghu Nandan Y
Department of General Surgery, Dr. B. R. Ambedkar
Medical College and Hospital, India.
Email: babbu5508@gmail.com
Received : Jul 23, 2022
Accepted : Oct 17, 2022
Published : Oct 24, 2022
Archived : www.jjgastro.com
Copyright : © Nandan YR (2022).
Abstract
Introduction: Intussusception of the bowel is defined as the telescoping of a proximal segment of the gastrointestinal tract within the lumen of the adjacent segment. This condition is frequent in children and presents with the classic triad of cramping abdominal pain, bloody diarrhea and a palpable tender mass. However, bowel intussusception in adults is considered a rare condition, accounting for 5% of all cases of intussusceptions and almost 1%-5% of bowel obstruction. Eight to twenty percent of cases are idiopathic, without a lead point lesion. Secondary intussusception is caused by organic lesions, such as inflammatory bowel disease, postoperative adhesions, Meckel’s diverticulum, benign and malignant lesions, metastatic neoplasms or even iatrogenically, due to the presence of intestinal tubes, jejunostomy feeding tubes or after gastric surgery. Computed tomography is the most sensitive diagnostic modality and can distinguish between intussusceptions with and without a lead point. Surgery is the definitive treatment of adult intussusceptions. Formal bowel resection with oncological principles is followed for every case where a malignancy is suspected. Reduction of the intussuscepted bowel is considered safe for benign lesions in order to limit the extent of resection or to avoid the short bowel syndrome in certain circumstances.
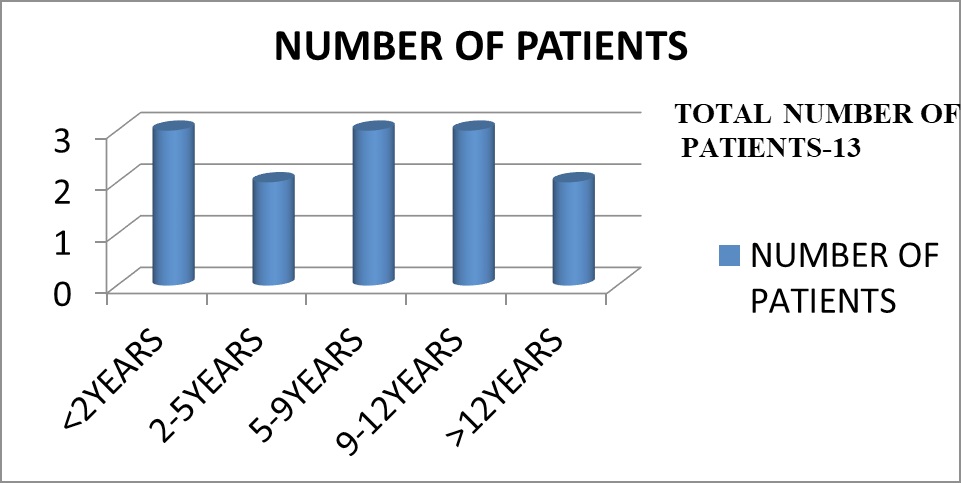
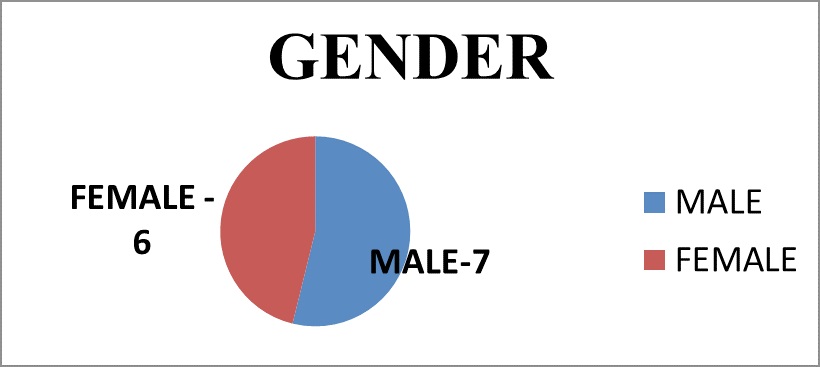
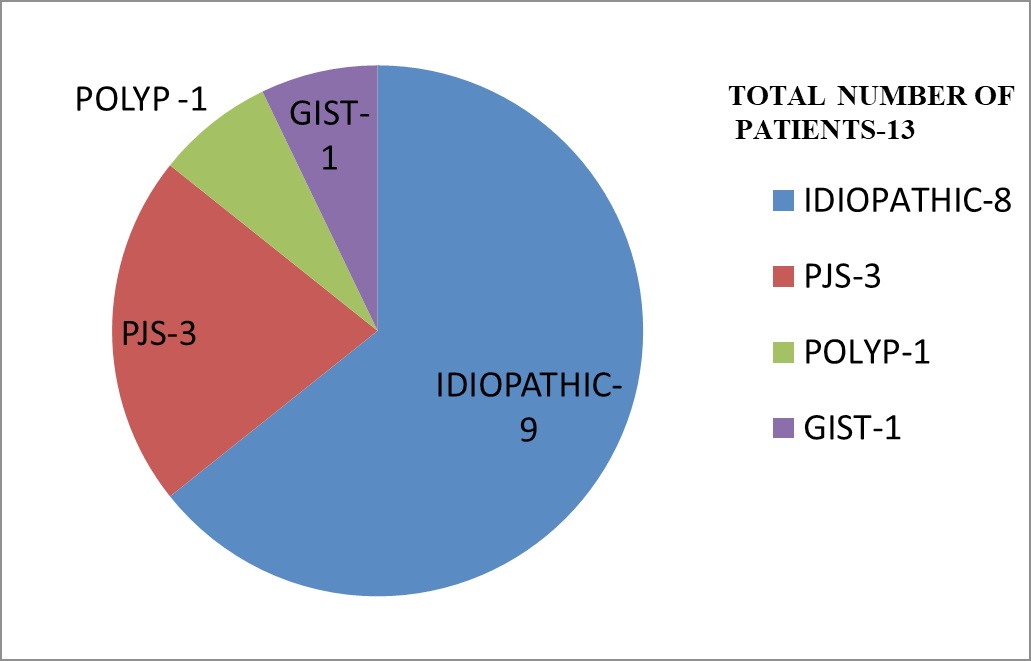
Methods: Study of 13 patients admitted between 1ST JUNE 2012 and 31 ST MAY 2014 At DR.B R Ambedkar Medical College.
Results: Of 13 cases, 2 cases underwent hydrostatic reduction one case failed and underwent emergency laparotomy and resection anastomosis,6 cases underwent operative reduction, 4 cases underwent resection anastomosis, 1 case of PJS underwent operative reduction and polypectomy, 1 case of PJS underwent resection anastomosis and polypectomy, 1 case of PJS refused surgery and expired.
Conclusion: Though hydrostatic /pneumatic reduction is the mainstay of treatment in developed countries in our country most cases are diagnosed and referred later than 72hrs Hence, nonoperative reduction may not be always be feasible in most of the patients in our setup and number of patients requiring resection and anastomosis, is high.In older patients of intussusception pathological lead points should be suspected.
Citation: Nandan YR, Rajeev N. Experience of intussusception at a tertiary care hospital: A prospective study. Japanese J Gastroenterol Res. 2022; 2(14): 1115.
Methodology
Methods of collection of data: Study of 13 patients admitted between 1 ST JUNE 2012 and 31 ST MAY 2014 at DR.B R Ambedkar Medical College.
Inclusion criteria: All cases of intussusception of all ages and gender presented to our hospital including those who refused surgery.
Results
Case details
Evaluation:
• Clinical Examination
• Erect X –Ray Abdomen
• Usg Abdomen
• Cect Abdomen
• Clinical Examination
• Erect X –Ray Abdomen
• Usg Abdomen
• Cect Abdomen
CLINICAL FEATURES |
NUMBER OF PTS |
PERCENTAGE |
Abdominal pain |
13 |
100% |
Abdominal mass |
5 |
38% |
“Red currant jelly” stools |
4 |
30% |
Vomiting |
7 |
53% |
Abdominal distention |
4 |
30% |
Hypovolemic shock |
2 |
15% |
Pallor |
4 |
30% |
Erect x –ray abdomen:
Erect x-ray abdomen was done to look for free air under diaphragm and to look for obstruction
Ultrasonography:
• All patients underwent USG
• Doppler was used to determine bowel ischemia; guides reduction decisions
• Ultrasonography was diagnostic in 93% of our cases
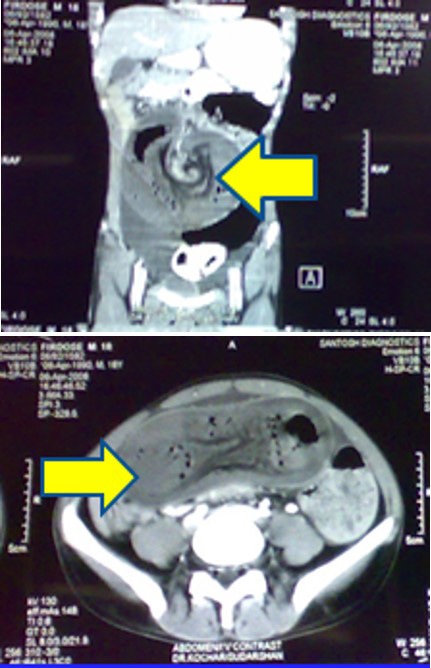
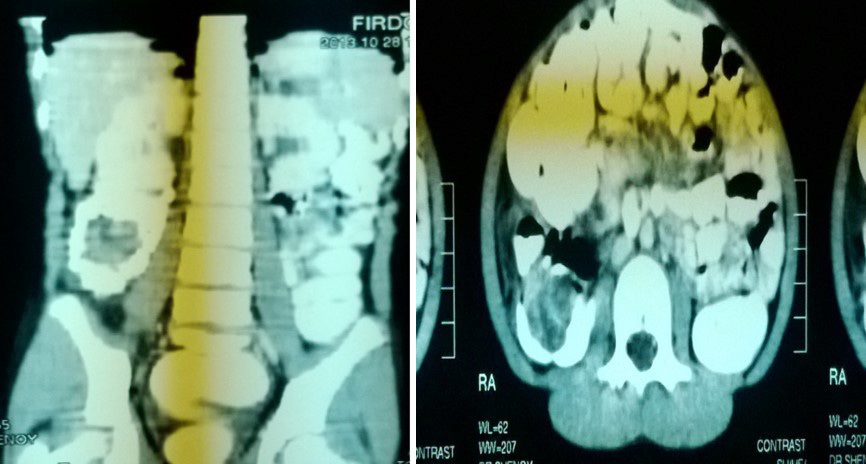
Computer tomograpahy:
• CT was done in 2 of our cases
• 1 case of PEUTZ JEGHERS SYNDROME
• 1 case was of chronic intussusception with benign polyp as lead point in ascending colon
Management:
• HYDROSTATIC SALINE REDUCTION:
• Patients of age <3 years presented with 72 hrs of duration underwent hydrostatic saline reduction under USG guidance.
• 2 cases- 1case failed and underwent emergency laparotomy and resection anastomosis.
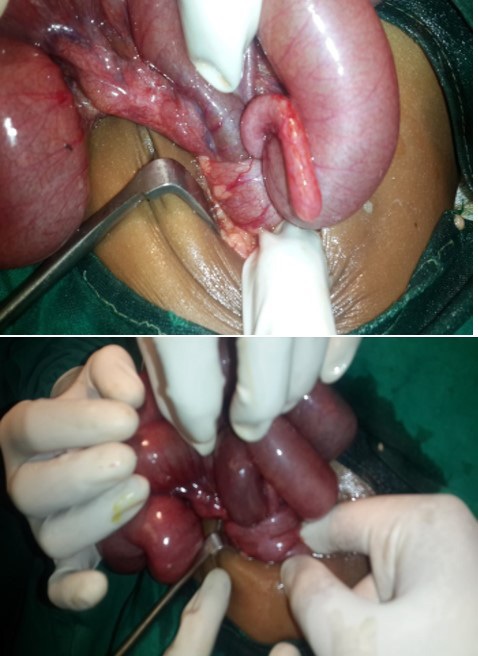
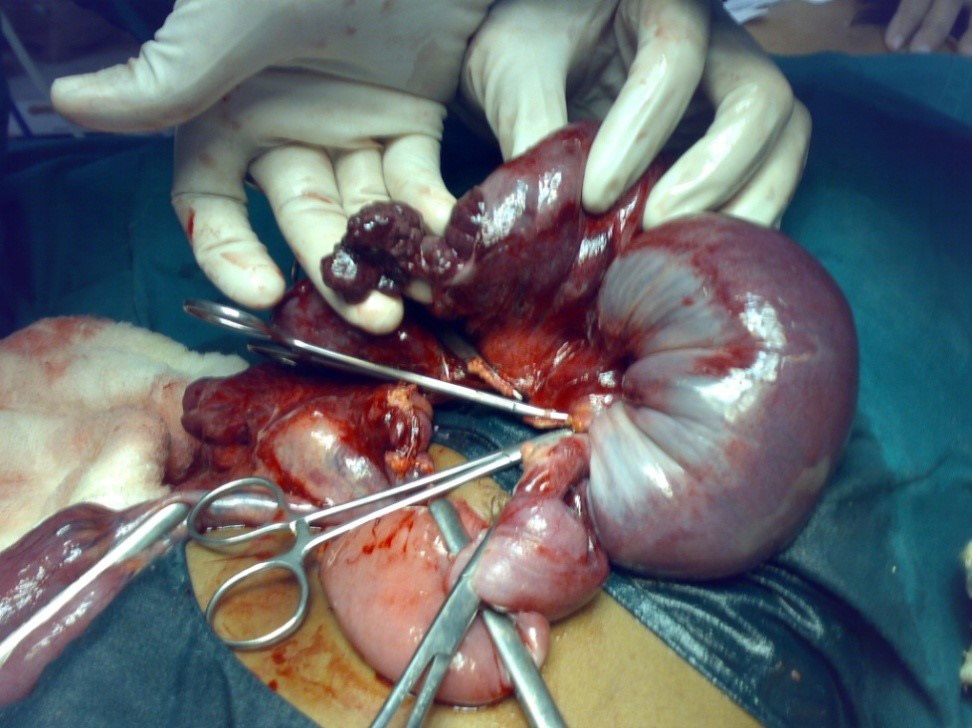
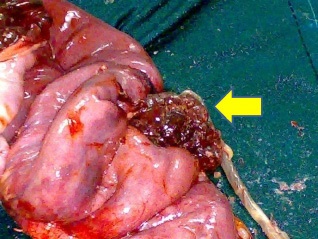
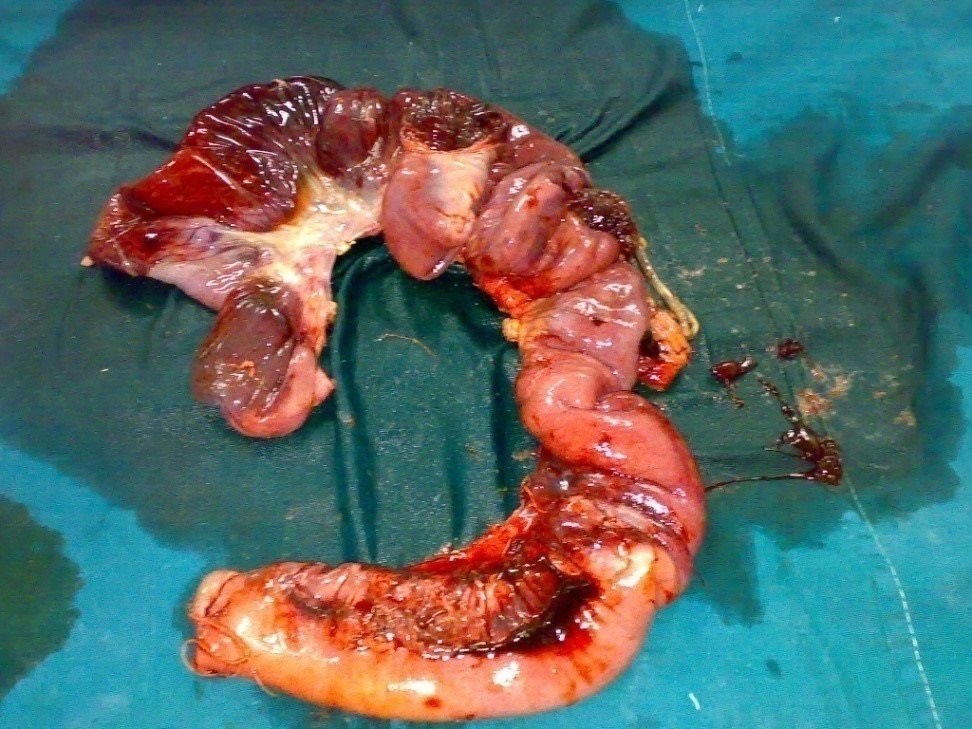
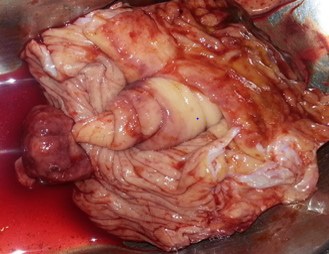
Peutz jeghers syndrome - per operative findings in the child
• Jejuno-ileal intusussception with multiple polyps in the jejunum.
• Gangrene of the bowel seen.
Peutz jeghers syndrome:
• Our case report-3 cases (family)
• 2 male-11,50 yrs (father)
• 1 female-8 years
PEUTZ JEGHERS SYNDROME(FAMILY)
11yrs |
8yrs |
50yrs(father) |
|
Vital Signs |
In shock |
WNL |
shock |
Muco-cutaneous Jn |
Hyperpigmented spots on both the lips & buccal mucosa |
Hyperpigmented spots present over buccal mucosa |
Hyperpigmented spots |
Per Abdomen |
Tender mass in the unbilical region with abdominal distension |
Tender mass in right hypochondrium |
abdominal distension |
Per rectal |
Red currant jelly stools |
WNL |
WNL |
USG |
Jejunoileal |
Ileocolic intussusception |
Ileocolic intussusception |
Xray Abdomen |
Multiple air fluid levels |
NOT DONE |
Multiple air fluid levels |
CT Scan Abdomen |
Jejunoileal intussusception |
NOT DONE |
NOT DONE |
management |
Operative reduction and Resection anastomosis |
Operative reduction and polypectomy |
refused |
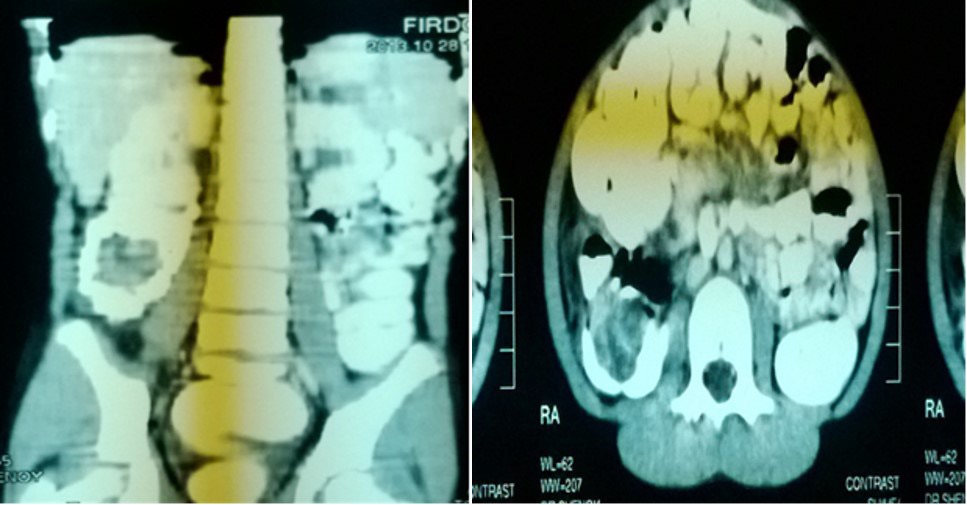
Chronic intussusception:
• 12 years old female patient presented with chronic abdominal pain since 6 months.
• USG ABDOMEN-WNL.
• CT ABDOMEN.
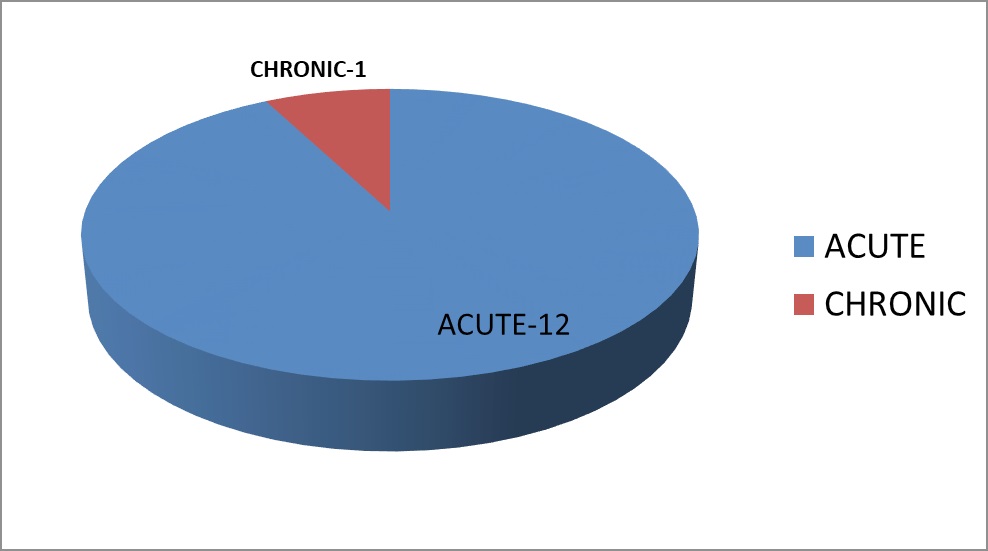
Our results:
• Of 13 cases, 2 cases underwent hydrostatic reduction one case failed and underwent emergency laparotomy and resection anastomosis.
• 6 cases underwent operative reduction.
• 4 cases underwent resection anastomosis.
• 1 case of PJS underwent operative reduction and polypectomy.
• 1 case of PJS underwent resection anastomosis and polypectomy.
• 1 case of PJS refused surgery and expired.
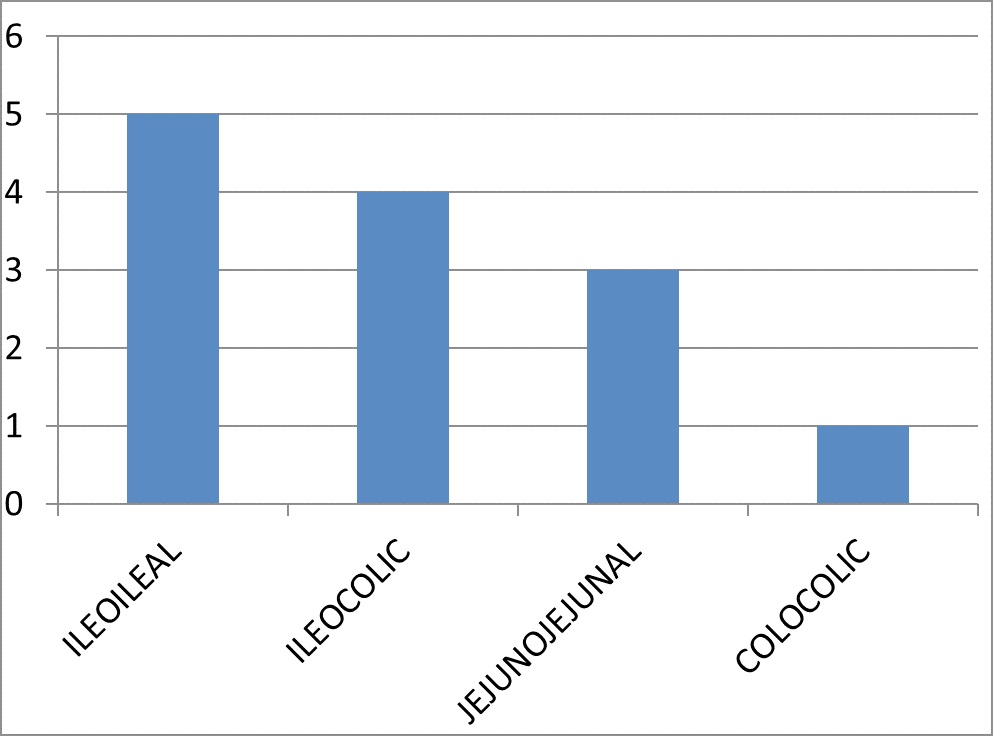
11313 CASES |
AGE AND SEX |
TYPE AND MANAGEMENT |
1 |
6MONTHS/F |
ILEOCOLIC -OPER REDUCTION |
2 |
6MONTHS/F |
ILEOCOLIC -FAILED HYDROSTATIC REDUCTION –OPER REDCUTION &RESECTION ANASTOMOSIS |
3 |
9MONTHS/M |
ILEOILEAL-OPER REDUCTION |
4 |
3 YEARS/M |
ILEOCOLIC-OPER REDUCTION |
5 |
4 YEARS/M |
ILEOCOLIC- HYDROSTATIC REDUCTION |
6 |
5 YEARS/M |
ILEOILEAL-OPER REDUCTION |
7 |
8 YEARS/M |
ILEOILEAL-OPER REDUCTION |
8 |
8 YEARS/F |
JEJUNOJEJUNAL-OPER REDUCTION&POLYPECTOMY AND ENTEROTOMY |
9 |
9 YEARS/M |
JEJUNOJEJUNAL-OPER REDUCTION |
10 |
11 YEARS/M |
JEJUNOJEJUNAL/PJS-OPER REDUCTION&RESECTION ANASTOMOSIS AND POLYPECTOMY |
11 |
12 YEARS/F |
CHRONIC INTUSSUSCEPTION WITH POLYP-RESECTION ANASTOMOSIS |
12 |
50 YEARS |
JEJUNOJEJUNAL/PJS-REFUSED SURGERY AND EXPIRED |
13 |
52 YEARS |
COLOCOLIC INTUSSUSCEPTION/GIST-RESECTION ANASTOMOSIS |
Discussion
Etiologies of intussusception:
Idiopathic:
• no defined lead point
• Association with viral illness (adenovirus)
• Hypertrophy of lymphoid tissue
Recognizable cause for lead point:
• Meckel’s diverticulum
• Intestinal polyp
• Enteric duplication
• Lymphoma
• Intramural hematoma
• Henoch-Schönlein purpura
Clinical presentation: Variable
Classic Triad: abdominal pain, currant jelly stool, palpable abdominal mass (<50%).
Complications:
• Typically do not occur within the first 24 hrs…
• Bowel obstruction
• Intestinal ischemia
• Perforation
• Shock
• Sepsis
• Dehydration
Thus we have a window of opportunity in which to treat by hydrostatic or pneumatic reduction procedure and avoid surgery.
Screening tools:
Abdominal radiograph
• Screen for other differential diagnosis and free air
• 45% sensitivity
Abdominal sonography
• Diagnostic accuracy near 100%, evaluation of reducibility, lead point, post reduction, ischemia
• Abdominal CT scan
• Accuracy approaching 100%; especially good for lead points
• High cost, risk of radiation, and risk of sedation in children make it unpractical
Abdominal ultrasound:
Replaced abdominal radiograph as primary screening modality
• Sensitivity 98 -100%; specificity 88 -100%
• Appearance: outer hypoechoic region surrounding an echogenic center or multiple concentric rings
• Use Doppler to determine bowel ischemia; guides reduction decisions
• Guide hydrostatic and pneumatic reduction
Reduction procedures:
• Barium enema: previous standard for Dx and reduction
• Risk of barium :peritonitis, infection, adhesions, radiation exposure with fluoroscopy, only see lumen
• US-guided Hydrostatic reduction No radiation, good visualization of intussusception & lead points
• Need sonographer
• Pneumatic reduction with fluoroscopic guidance
• Quick, safe, clean (less fecal spillage), cheap
• Radiation exposure, cannot detect lead points well, only see intraluminal content
• US-guided Pneumatic reduction
• No radiation, confirm dx, highest successful reduction rate (92%), quick and clean, can see lead points well (but not all)
• Air blocks US beam; difficult to see ileocecal valve and residual intussusceptions
Contraindications to reduction procedures:
• Dehydration
• Peritonitis
• Shock
• Sepsis
• Free air on radiograph
• Stabilize then treat surgically
Complications of reduction:
• Perforation rate of 0.8%
• Recurrence -10%
• 50% will occur within 48 hrs
• Repeat enemas are safe and effective
Reduction guidelines
• Rule of Three’s for Barium
• 3 attempts
• 3 min duration
• Liquid enema bag 3 feet above fluoroscopy table (5 feet if using water-soluble contrast)
• Air Enema Ensure maximal pressures <120 mm Hg at rest
Success of reduction depend On…
• Short duration of symptoms (<24-48 hrs)
• Adequate hydration
• Age (older than 3 months)
• Absence of small-bowel obstruction
• Absence of trapped intra peritoneal fluid
• Absence of enlarged lymph nodes in the intussusceptum
• Adequate blood flow
• Location other than the rectum (rectum only 25% success)
Peutz-jeghers syndrome
• PJS is a rare familial disease with a 4 fold increased risk of intestinal and extra intestinal malignancies.
• PJS presenting as intussusception though common in children is rare in adults representing only 1% of bowel obstruction.
• Mucocutaneous pigmentations caused by melanin aggregation is seen in 93% of patients in infancy with the pigmentation fading with age.
• Small bowel polyps can reach up to 100s in number.
• Lack of adequate follow up and cancer surveillance is a potential pitfall
• Every 1st degree relative of PJS patient should be screened for polyps.
• Genetic counselling is recommended for patients and their relatives.
• Morbidity includes small intestinal obstruction and intussusception (43%), abdominal pain(23%), hematochezia(14%).
• Refrain from excessive resection of the bowel as PJS patients may be subjected for repeated laparotomies & resection anastomosis due to intussusception.
• Polyps found intraoperatively to be removed by enterotomy
Conclusion
Though hydrostatic /pneumatic reduction is the mainstay of treatment in developed countries, in our country most cases are diagnosed and referred later than 72hrs
• Hence, non-operative reduction may not be always be feasible in most of the patients in our setup and number of patients requiring resection and anastomosis, is high
• In older patients of intussusception pathological lead points should be suspected
References
- Felix EL, Cohen MH, Bernstein AD, Schwartz JH. Adult intussusception; case report of recurrent intussusception and review of the literature. Am J Surg 1976; 131: 758-761.
- Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, Kohneh-Sharhi N, et al. Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis 2006; 21: 834-839.
- Wolff BC, Boller AM. Large bowel obstruction. In: Cameron JL. Current surgical therapy. Philadelphia: Mosby Elsevier 2008.
- Wang LT, Wu CC, Yu JC, Hsiao CW, Hsu CC, Jao SW. Clinical entity and treatment strategies for adult intussusceptions: 20 years’ experience. Dis Colon Rectum 2007; 50: 1941-1949.
- Lin BC, Lien JM, Chen RJ, Fang JF, Wong YC. Combined endoscopic and surgical treatment for the polyposis of Peutz-Jeghers syndrome. Surg Endosc 2000; 14: 1185-1187.
- Gonzalez AM, Clapp B. Laparoscopic management of small bowel intussusception in a 16-year-old with Peutz-Jeghers syndrome. JSLS 2008; 12: 332-334.
- Lin MW, Chen KH, Lin HF, Chen HA, Wu JM, Huang SH. Laparoscopy-assisted resection of ileoileal intussusception caused by intestinal lipoma. J Laparoendosc Adv Surg Tech A 2007; 17: 789- 792.
- Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV. Minimal access surgery for adult intussusception with subacute intestinal obstruction: a single center’s decade long experience. Surg Laparosc Endosc Percutan Tech 2007; 17: 487-491.
- Chuang Ch, Hsieh C, Lin Ch, Yu J. Laparoscopic management of sigmoid colon intussusception caused by a malignant tumor: case report. Rev Esp Enferm Dig 2007; 99: 615-616.
- Ishibashi Y, Yamamoto S, Yamada Y, Fujita S, Akasu T, Moriya Y. Laparoscopic resection for malignant lymphoma of the ileum causing ileocecal intussusception. Surg Laparosc Endosc Percutan Tech 2007; 17: 444-446.
- Akatsu T, Niihara M, Kojima K, Kitajima M, Kitagawa Y, Murai S. Adult colonic intussusception caused by cecum adenoma: successful treatment by emergency laparoscopy: report of a case. Surg Today 2007; 37: 694-697.
- Tsushimi T, Matsui N, Kurazumi H, Takemoto Y, Oka K, Seyama A, Morita T. Laparoscopic resection of an ileal lipoma: Report of a case. Surg Today 2006; 36: 1007-1011.
- McKay R. Ileocecal intussusception in an adult: the laparoscopic approach. JSLS 2006; 10: 250-253.
- Wu JM, Lin HF, Chen KH, Tseng LM, Huang SH. Laparoscopic diagnosis and treatment of small bowel obstruction caused by postoperative intussusception. J Laparoendosc Adv Surg Tech A 2006; 16: 137-140.
- Park KJ, Choi HJ, Kim SH, Han SY, Hong SH, Cho JH, Kim HH. Sigmoidorectal intussusception of adenoma of sigmoid colon treated by laparoscopic anterior resection after sponge-on-thestick-assisted manual reduction. World J Gastroenterol 2006; 12: 146-149.
- Jelenc F, Brencic E. Laparoscopically assisted resection of ascending colon lipoma causing intermittent intussusception. J Laparoendosc Adv Surg Tech A 2005; 15: 173-175.