Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 2
Torsion of congenital ovarian cyst in association with mid-gut volvulus: A rare presentation
Ahmed Elrouby
Associate Professor of Pediatric Surgery, Faculty of Medicine, Alexandria University, Egypt.
*Corresponding Author : Ahmed Elrouby
Associate Professor of Pediatric Surgery, Faculty of
Medicine, Alexandria University, Egypt.
Email: elroubypaedo@yahoo.com
Received : Sep 05, 2022
Accepted : Oct 06, 2022
Published : Oct 13, 2022
Archived : www.jjgastro.com
Copyright : © Elrouby A (2022).
Abstract
Midgut volvulus is a life-threatening condition that can lead to bowel ischemia and devastating results with high mortality incidence. An ovarian cyst can be accidentally discovered antenatal or postnatal and can be asymptomatic, mass presentation, or complicated presentation as torsion. The association of midgut volvulus and an ovarian cyst is exceptional. We report a case with an antenatal diagnosis of a right ovarian cyst that presented to our emergency department with acute abdomen combined with upper and lower GIT bleeding. Clinical examination revealed a tender and distended abdomen. The patient underwent an emergency laparotomy that revealed torsion of a right ovarian cyst with mid-gut volvulus, gangrenous bowel with multiple perforations, and feculent peritoneal collection. Resection of the entire gangrenous perforated intestine with the construction of a double-divided ileostomy was done with excision of the ovarian cyst.
Keywords: Midgut volvulus; Ovarian cyst; Ovarian torsion; Laparotomy
Citation: Elrouby A. Torsion of congenital ovarian cyst in association with mid-gut volvulus: A rare presentation. Japanese J Gastroenterol Res. 2022; 2(13): 1111.
Introduction
Midgut volvulus is a condition in which a portion of the bowel twists upon itself. The most common causes include malrotation and intestinal atresia. If midgut volvulus occurs with normal mesenteric fixation and no malrotation, it is termed primary midgut volvulus. Unrecognized midgut volvulus leads to bowel ischemia with varying degrees of bowel necrosis. The incidence of midgut malrotation in the pediatric age group is about 1 in 500 live births [1].
On the other hand, ovarian cysts are common in fetuses and neonates. Although the true incidence of fetal ovarian cysts is unknown, they have been detected in approximately 30 to 70 percent of fetuses on routine antenatal ultrasonography. The incidence of clinically important ovarian cysts is estimated to be 1 in 2500. The risk of torsion increases with the presence of an ovarian cyst that exceeds 5 cm. ovarian torsion accounts for approximately 3% of all cases of children with acute abdominal pain that requires immediate surgical intervention [2].
The combination of mid-gut volvulus, and ovarian cyst, is not reported so we present here a rare case of congenital ovarian cyst associated with mid-gut volvulus. A review of the diagnosis and management is subsequently carried out.
Case report
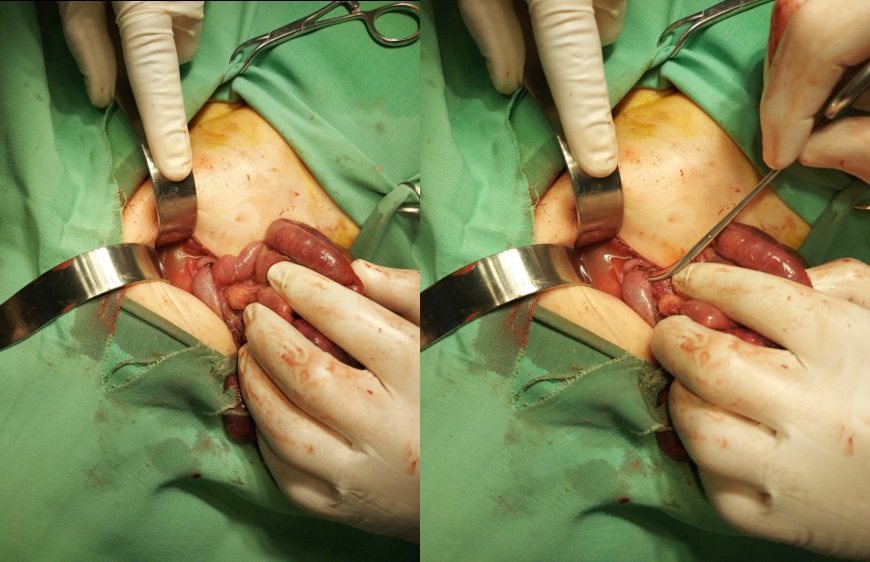
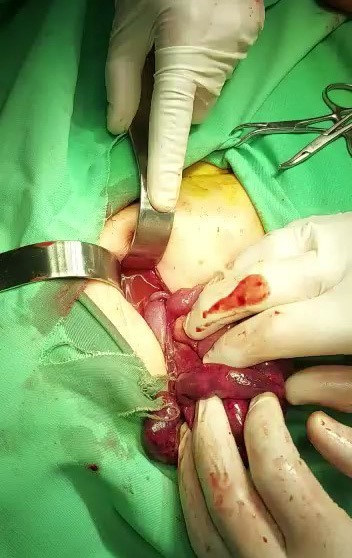
A female neonate was referred to our department with acute abdomen, upper and lower GI bleeding, with a prenatal history of undifferentiated abdominal cyst measuring about 3 x 4 cm. Exploration revealed torsion of a right ovarian cyst with mid-gut volvulus (Figure 1), gangrene with multiple perforations, and feculent peritoneal collection (Figures 2,3). The decision was taken to do resection of the entire gangrenous perforated intestine with construction of a double-divided ileostomy about 20 cm from the duodeno-jejunal junction leaving about 15 cm from the ileocecal valve in association with excision of the cyst (Figure 4).
Peritoneal lavage with warm saline and betadine followed by insertion of an intra-abdominal drain with the two edges of the ileostomy fixed to the two lateral edges of the wound with en mass closure of the abdominal wound. The patient was transferred to the neonatal intensive care unit on IV fluids, close monitoring of the input and output schedule, and regular wound care with local betadine disinfectant and antibiotic.
Bilious suction from the nasogastric tube stopped on the 3rd postoperative day when it was removed in association with the abdominal drain. Passage of soft stool was observed from the 3rd post-operative day when the patient started oral intake. The patient tolerated oral feeding with the passage of undigested milk from the stoma depending mainly on the parenteral fluid supply to keep homeostasis with a smooth postoperative period. Partial dehiscence of the abdominal wound with skin inflammation was observed with regular dressing. The patient is still admitted as she depends mainly on parenteral fluid supply.
Discussion
Neonatal Midgut volvulus is an uncommon disease that may be seen in infants and older children [3,4]. Early diagnosis of such pathology is very important especially in neonates as it usually ends with bowel ischemia and gangrene in neglected cases with very high morbidity & mortality; so, early diagnosis with urgent intervention is crucial to decrease morbidity and mortality [5].
Abnormal positioning of the bowel loops in the peritoneal cavity during the intrauterine life is the direct cause of volvulus [6]. It is caused by defective rotation of the primitive intestinal loop around the axis of the superior mesenteric artery during embryogenesis [7] that leads to short mesenteric root leading to twisting of the bowel loops around its axis leading to midgut volvulus [8].
Currently, the positive diagnosis of midgut volvulus can be detected antenatally. The imaging workup of suspected neonatal volvulus classically consists of plain abdominal radiograph and/or contrast studies [9]. Ultrasound can be the first non-invasive, radiation-free, mostly available, and inexpensive imaging modality to start with. It can give a clue about the abnormal position of the superior mesenteric artery and vein; as in 60% of individuals the relative positions of both vessels are reversed in midgut malrotation revealing the classic sonographic appearance of midgut volvulus: “whirlpool sign” [10,11]. This Whirlpool is created by the superior mesenteric vein and mesentery wrapping around the artery in a clockwise direction [7,12].
The findings of radiographs are not so specific, but they can give clues about proximal bowel obstruction as well as the abnormal location of the small and large intestine. Conventionally, the diagnosis of malrotation is made by upper gastrointestinal contrast studies documenting the position of the duodenojejunal flexure. Patients with malrotation will have a duodenojejunal flexure to the right of or below the normal position that is to the left of vertebral pedicles at the level of the duodenal bulb on an anteroposterior view of a well-positioned patient [13].
The associated obstruction may be complete or partial so the further passage of contrast to the small bowel may not be sometimes seen. The pathognomonic feature of volvulus on the upper GI series is the “corkscrew pattern” of the twisted duodenum and jejunum [14].
Ovarian and genital tract abnormalities constitute approximately 20% of all abdominal masses in the neonate. These cysts vary in size; they can be simple or complex and are commonly unilateral. Intrauterine and neonatal complications such as torsion and rupture may occur, and treatment options vary from conservative management to antenatal aspiration, early delivery, and neonatal surgery [15].
In our case, surgical management was the only therapeutic option due to the acute presentation. The decision to excision the ovary was taken as it was complicated with volvulus also resection anastomosis option for bowel management was rejected and instead decision of making stoma was taken as the feculent material was all over the abdomen.
Conclusion
Congenital ovarian cysts have to be treated early and promptly to avoid the development of intra-abdominal complications which increase postoperative morbidity and mortality.
Declarations
Conflict of interest: There was no conflict of interest to declare.
Funding sources: Threre was no funding sources for our manuscript.
Acknowledgment: The authors acknowledge all staff members of our pediatric surgery unit for their great support.
Funding: Our manuscript didn’t receive any fund.
References
- Gourishetti S, DeMeo SD. Neonatal segmental small bowel volvulus with normal intestinal rotation. J Pediatr Surg Case Reports. 2021; 64: 101721.
- Breech LL, Hillard PJA. Adnexal torsion in pediatric and adolescent girls. Curr Opin Obstet Gynecol. 2005; 17: 483-489.
- Sivitz AB, Lyons R. Mid-Gut Volvulus Identified by Pediatric Emergency Ultrasonography. J Emerg Med. 2013; 45: e173-4.
- Kanellos-Becker I, Bergholz R, Reinshagen K, Boettcher M. Early prediction of complex midgut volvulus in neonates and infants. Pediatr Surg Int. 2014; 30: 579-586.
- Lampl B, Levin TL, Berdon WE, Cowles RA. Malrotation and midgut volvulus: a historical review and current controversies in diagnosis and management. Pediatr Radiol. 2009; 39: 359-366.
- Applegate KE, Anderson JM, Klatte EC. Intestinal Malrotation in Children: A Problem-solving Approach to the Upper Gastrointestinal Series. RadioGraphics. 2006; 26: 1485-1500.
- Epelman M. The Whirlpool Sign. Radiology. 2006; 240: 910-911.
- Peterson CM, Anderson JS, Hara AK, Carenza JW, Menias CO. Volvulus of the Gastrointestinal Tract: Appearances at Multimodality Imaging. RadioGraphics. 2009; 29: 1281-1293.
- KEN KIMURA MD, VERA LOENING-BAUCKE M. Bilious Vomiting in the Newborn: Rapid Diagnosis of Intestinal Obstruction. Am Fam Physician. 1: 2791-2798.
- Zerin JM, DiPietro MA. Mesenteric vascular anatomy at CT: normal and abnormal appearances. Radiology. 1991; 179: 739-742.
- Zerin JM, DiPietro MA. Superior mesenteric vascular anatomy at US in patients with surgically proved malrotation of the midgut. Radiology. 1992; 183: 693-694.
- Rokade ML, Yamgar S, Tawri D. Ultrasound “Whirlpool Sign” for Midgut Volvulus. J Med Ultrasound. 2011; 19: 24-26.
- Birajdar S, Rao SC, Bettenay F. Role of upper gastrointestinal contrast studies for suspected malrotation in neonatal population. J Paediatr Child Health. 2017; 53: 644-649.
- Ortiz-Neira CL. The Corkscrew Sign: Midgut Volvulus. Radiology. 2007; 242: 315-316.
- Sintim-Damoa A, Majmudar AS, Cohen HL, Parvey LS. Pediatric Ovarian Torsion: Spectrum of Imaging Findings. Radio Graphics. 2017; 37:1892-1908.