Japanese Journal of Gastroenterology Research
Research Article - Open Access, Volume 2
Histopathological patterns of pancreatic malignancy among Afro Sudanese patients: A step towards preliminary database in a developing country
Nassir Alhaboob Arabi Mohammad1*; Abdulmagid M Musaad1; Babiker Abdelaziz Babiker Ibrahim2; Modather MohamedEltayeb Salih2; Mohamed Mustafa Ismail Elhaj Ahmed2; Hayat Tarig Mohamed Zeyada2; Asma Ismail Zainalabdin Ahmed2; Ayah Gafar Yassin Abdusayed2; Mohamed Eltayeb Abdelrahman Naiem3; Elsaggad Eltayeb Ahmed4
1Department of GI & HPB Surgery, Ibn Sina specialized hospital, Khartoum, Sudan.
2Faculty of Medicine, Omdurman Islamic University, Khartoum, Sudan.
3Faculty of Medicine - University of Khartoum, Khartoum, Sudan.
4Associate professor of surgery, faculty of medicine, Al Nilin University Khartoum, Sudan.
*Corresponding Author : Arabi Mohammad NA
Consultant Surgeon, Associate Professor of Surgery, OIU, Department of GI & HPB Surgery, Ibn Sina Specialized hospital, Khartoum, Sudan.
Email: nassir_alhaboob@yahoo.com
Received : Jul 06, 2021
Accepted : Jul 27, 2022
Published : Aug 03, 2022
Archived : www.jjgastro.com
Copyright : © Mohammad NAA (2022).
Abstract
Background: Pancreatic cancer mortality is considered the fourth commonest international cause of cancer-related death. Most available treatment modalities are ineffective, contributing to poor prognosis in this aggressive type of cancer. Surgical resection is the only curative treatment, and due to low resources and underprovided care in Africa, more than 80% of patients are not suitable for curative intervention at presentation. Furthermore, data on the histopathology of pancreatic tumors from developing countries are lacking. This study aims to identify the most common histopathological patterns among African Sudanese patients with malignant pancreatic neoplasms and establish a reference database for more studies.
Methods: It is retrospective, cross-sectional, descriptive observational hospital-based study on Ninety-five patients’. The variables like age, gender, histopathological diagnosis were measured. Frequencies and proportions were used to describe patient demographics, variables such as age were described with mean, all tests were two-tailed. Data were analyzed using SPSS software (version 25), and statistics were considered significant when P-value <0.05.
Results: The mean age was 56.7 years (sd±14.5). Fifty-four were males, and the male to female ratio was 1.3:1. There were 78.9% (n=75) patients had exocrine tumors while 19% (n=18) had neuroendocrine tumors and 2.1% (n=2) with non-epithelial lymphoma tumors. The Commonest site of tumors was the pancreatic head in 84.9% (n=79). In those 75 patients with exocrine tumors, ductal adenocarcinoma 81.3% (n=61), followed by cystadenocarcinoma 8% (n=6).
Conclusion: Pancreatic ductal adenocarcinoma is the most common histopathological subtype of pancreatic neoplasms among the Afro-Sudanese population, and neuroendocrine tumors were more prevalent in younger patients.
Keywords: Pancreatic Cancer; Histopathology pattern; Pancreatic Adenocarcinoma; PNETs; Neuroendocrine pancreatic tumors; Africa; Sudan; Malignant pancreatic neoplasms.
Abbreviations: DM: Diabetes mellitus; PDAC: Pancreatic ductal adenocarcinoma; PNETs: Pancreatic euroendocrine tumors; FNAC: Fine Needle Aspiration Cytology; ERCP: Endoscopic Retrograde Pancreatic-cholangiography; LAB: Laboratory; HPB: Hepato-pancreatic-biliary; VIP: vasoactive intestinal polypeptide.
Citation: Mohammad NAA, Musaad AM, Ibrahim BAB, Salih MME, Ahmed MMIE, et al. Histopathological patterns of pancreatic malignancy among Afro Sudanese patients: A step towards preliminary database in a developing country. Japanese J Gastroenterol Res. 2022; 2(2): 1101.
Background
Several cellular types form the pancreas, resembling a mixture of the two major exocrine and endocrine glandular components [1]. The exocrine component produces a combination of essential digestive enzymes and electrolytes-rich pancreatic juice [2], while the endocrine counterpart contains glandular cells responsible for anabolic and catabolic hormones production such as insulin and glucagon regulating carbohydrates metabolism [3]. The majority are exocrine pancreatic tumors with adenocarcinomas resembling almost ninety percent [4,5], followed by mucinous tumors, which account for less than a tenth of all pancreatic tumors [6]. On the other hand, tumors that arise from pancreatic endocrine cells are less common, accounting for less than 5% of all pancreatic tumors representing insulinomas, gastrinomas, VIPoma, and somatostatinoma [7]. Pancreatic malignancy is considered the fourth communal etiology of cancer-related death worldwide [8]. Furthermore, it is an aggressive type of cancer, and most of the available treatment modalities are ineffective, contributing to the poor overall disease prognosis. The only curative treatment is surgical resection; unfortunately, more than 80% of patients are not suitable candidates for curative resection since they present with a locally advanced or metastatic pancreatic disease at the time of diagnosis [9]. Pancreatic cancer commonly affects the male gender, usually above 55 years of life [10,11], and has a bleak prognosis with a virtual 5-year survival rate of only 8.2% [1]. In addition, the lack of screening methods for the early detection of pancreatic cancer has made the issue more complicated [12].
Data on histopathology of pancreatic tumors in the global literature from developing countries are scarce. Besides, there have been noticeable changes in the population’s demography, habits, and pathology. Therefore, our study’s primary purposes are to identify the most common histopathological patterns among Sudanese patients with pancreatic neoplasms and establish a preliminary database facilitating more future researches and studies.
Patients and methods
This study was conducted at Ibn Sina specialized hospital in Khartoum, the national gastrointestinal and hepato-pancreaticobiliary diseases center in Sudan; it is a retrospective, crosssectional, descriptive observational hospital-based study. Ninety-five patients’ clinicopathological information after being diagnosed with pancreatic cancer and receiving treatment in two years were collected and analyzed. The variables were: 1) age, 2) gender, 3) demography or region, 4) anatomical site of pancreatic tumor, and 5) histopathological diagnosis and variant using datasheet forms. It included all patients with confirmed histopathological diagnoses. Ninety-five patients met the inclusion criteria. Statistical analysis using (IBM SPSS version 25) was achieved; frequencies and proportions were used to describe patient demographics, variables such as age were described with mean, all tests were two-tailed, and statistics were considered significant when P-value < 0.05.
Results
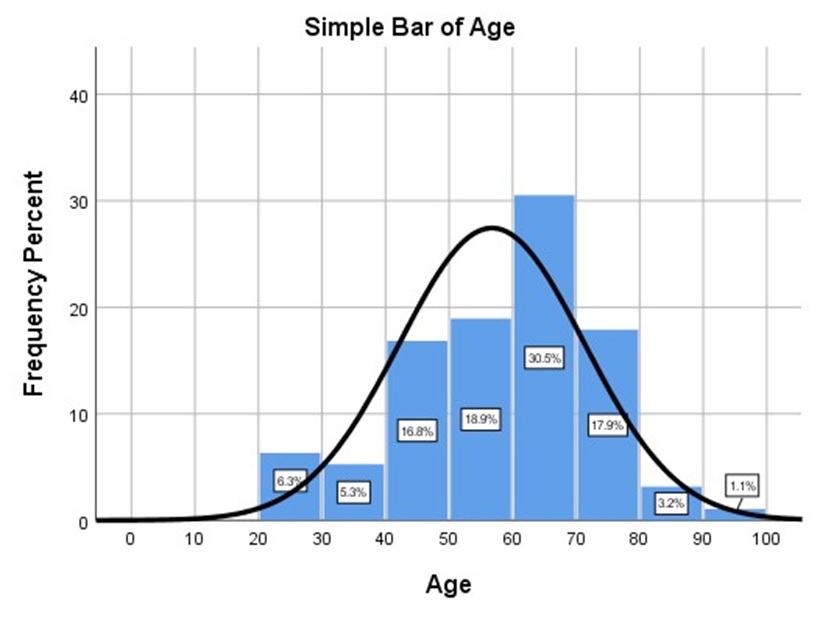
The mean age at diagnosis was 56.7 years (SD±14.5) (figure 1, table 1). Among them, 54 were males, male: female ratio was 1.3 to 1 (table 1). Thirty-two (33.7%) Histological examination of pancreatic tumors revealed 78.9% (n=75) of the patients with exocrine tumors, while 19% (n=18%) had neuroendocrine tumors and 2.1% (n=2) with non-epithelial lymphoma tumors (table 1). The most common anatomical location of tumors was the head of the pancreas, with an incidence of 84.9% (n=79). Metastatic disease was identified in 38.9 % (n=37) patients and principally metastasis to the liver. Distant metastases and locally advanced disease accounted for 67.4% at the time of diagnosis. Surgical resection was performed in 43 patients; 39 had Whipple’s operation, two received distal pancreatectomy, and two had segmental pancreatectomy. The remaining were deemed irresectable and assigned for palliative care. Exocrine tumors were diagnosed in 75 patients, and the most common histological type was ductal adenocarcinoma in 81.3% (n=61) patients, followed by cystadenocarcinoma in 8% (n=6) patients (Table 2). The mean age at diagnosis was 58.5years (SD±13.9) with a Male: Female ratio of 1.3 to 1 (table 1). Neuroendocrine tumors were identified in eighteen patients, with a mean age of 50 years (SD± 16.07) and a Male to Female ratio of 1.6:1 (table 1).
Table 1: Classification and demographics of patients with pancreatic tumors.
Type of tumor |
N |
% |
|
Epithelial |
Exocrine |
75 |
78.9 |
Neuro-endocrine |
18 |
19 |
|
Non-epithelial |
Lymphoma |
2 |
2.1 |
TOTAL |
95 |
100 |
|
AGE (years) |
Exocrine |
neuroendocrine |
Overall |
Mean |
58.5 |
50.2 |
56.7 |
Median |
60 |
56 |
60 |
Std. Deviation |
13.93 |
16.07 |
14.54 |
Gender |
|
|
|
Male |
43 (57.3%) |
11 (61%) |
54 (56.8%) |
Female |
32 (42.7%) |
7 (39%) |
41 (43.2%) |
Table 2: Histopathological types of exocrine tumors.
Histological Type |
N |
% |
Ductal adenocarcinoma |
61 |
81.3 |
Cyst adenocarcinoma |
6 |
8 |
Intraductal papillary mucinous neoplasm |
2 |
2.7 |
Cystadenoma |
3 |
4 |
Acinar cell carcinoma |
1 |
1.3 |
Mixed acinar, ductal Adenocarcinoma |
1 |
1.3 |
Solid pseudopapillary neoplasm |
1 |
1.3 |
Total |
75 |
100 |
Discussion
Pancreatic cancer is considered a challenging malignancy with an increasing incidence and high mortality. Pancreatic cancer is the second leading cause of cancer-related death [13]. The ultimate treatment modality is oncological surgical resection with R0 intent; unfortunately, the overall prognosis is poor due to its aggressive nature; most treatment modalities are ineffective. Carrara S reported that more than 80% of patients are locally advanced or metastatic pancreatic cancer at the time of diagnosis [9], compared to our results that found patients with locally advanced pancreatic cancer and distant metastasis account for 67.4% at the time of diagnosis. The early detection of environmental and personal risk factors for pancreatic cancer include advancing age, cigarette smoking, passive tobacco smoke exposure, obesity, and inherited familial cancers syndromes, could reduce mortality [14]. Statewide tumor registry found that adenocarcinoma was the most common pancreatic neoplasm, 89.9% (13,657/15,185 patients) it was 19 times more common than the next most common cancer type [15]. Other studies revealed that 90% of exocrine pancreatic tumors were adenocarcinomas [4,5], followed by mucinous tumors, which account for less than 10% of all pancreatic tumors [6]. In 2006, the American Cancer Society reported little change in the incidence of pancreatic cancer; given that the preponderance of pancreatic cancer is adenocarcinoma [16], we had similar results showed that ductal adenocarcinoma is still the most common type of pancreatic tumors (81.6%) followed by cystadenocarcinoma (8%), while there is an uprising in neuroendocrine tumors (19%).
In two separate studies, Ilic M and Yadav D showed that the median age of diagnosis in a patient with pancreatic cancer is 71 years, and there is a link between the risk of developing pancreatic cancer and advanced age. More than 90% of cases were diagnosed after 55 years [10,11]. Moreover, a 16-Year Review of Statewide Tumor Registry found that the mean age at presentation was similar for tumor types, 69.2 years old, except for endocrine neoplasms occurring at a younger age of 58.5 years [15]. There is an alarming trend that our patients had a younger age with a mean age of 56.7 years (sd±14.5), and especially for PNETs with a mean age of 50 years, this trend has to be investigated further due to adverse socio-economic effects on the individual, community, and country as a whole.
A meta-analysis on Global incidence and mortality of pancreatic diseases reported incidence of pancreatic cancer was 9.79 cases (7.20–13.32) per 100,000 person-years among men and 8·08 cases (5.24–12.45) per 100,000 person-years among women (17). Furthermore, Priya K Simoes showed that global incidence rates per 100,000 of 4.9 for men and 3.6 for women, consistent across all regions [18]; we share the same results with giving male to female ratio of 1.3 to 1 for PDAC and a higher ratio of 1.6 to 1 for PNETs. Furthermore, a population-based study found that PNETs had a significantly younger median age at diagnosis (61y vs. 69 y) and had a higher proportion of males (55.2% vs. 51.6%) when compared to pancreatic adenocarcinomas [19].
Conclusion
This study provides a cornerstone database in a developing country demonstrating the current histopathological pattern of malignant pancreatic tumors in Sudan, supporting future studies and data extraction using the international health systems regulations. Ductal adenocarcinomas are still the most prevalent histopathological types among pancreatic neoplasms, and there is an observed uprising in neuroendocrine tumors. Our patients tend to be younger than worldwide with a mean age of the 50s, and males are slightly more affected than females, probably due to an upsurge in the risk factors (smoking and DM) in our region, which need further studies and investigations.
Declarations
Recommendations: More research needs to be done on pancreatic neoplasms in our region to build an extensive database for our health system and comparison with international systems.
Acknowledgment: We want to thank the Head of Medical Records and our laboratory staff for their help and the medical team in Ibn Sina specialized hospital.
Authors contributions: All authors have recited and approved the manuscript.
NAAM: Design, Questionnaire Development, Data Collection, Data Analysis, Drafted manuscript, Manuscript Review.
AMM: Conception, Design, Manuscript Review.
BABI, MMIEA, HTMZ, AIZA, and AGYA: Conception, Questionnaire Development, Data collection & analysis,
MEAN and EEA: Drafted Manuscript, Manuscript Review.
Funding: All authors declare that they have no funding and it is not applicable.
Availability of data and materials: All data and material are available when they needed upon request through corresponding author.
Ethics approval and consent to participate: Ethical clearance was attained from the ethical committee and research at Ibn Sina Specialized Hospital – Khartoum, Sudan. Written informed consent was obtained from the patients for publication and any accompanying materials. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests: All authors declare that they have no competing interests.
References
- Fesinmeyer, Austin MA, Li CI, De Roos AJ, Bowen DJJCE, Biomarkers P. Differences in survival by histologic type of pancreatic cancer. 2005; 14: 1766-73.
- Hollingsworth MAJAotNYAoS. Proteins Expressed by Pancreatic Duct Cells and Their Relatives. 1999; 880: 38-49.
- Girolami U, Anthony D, Frosch M Cotran RS, Kumar V, Collins T. Robbins pathologic basis of disease. Philadelphia. PA: WB Saunders; 1999.
- Cowgill SM, Muscarella PJTAjos. The genetics of pancreatic cancer. 2003; 186: 279-86.
- Li D, Jiao LJIjogc. Molecular epidemiology of pancreatic cancer. 2003; 33: 3-13.
- Tenner S, Carr-Locke DL, Banks PA, Brooks DC, Van Dam J, Farraye FA, et al. Intraductal mucinhypersecreting neoplasm” mucinous ductal ectasia”: endoscopic recognition and management. 1996; 91.
- Mullan MH, Gauger PG, Thompson NWJAjos. Endocrine tumours of the pancreas: review and recent advances. 2001; 71: 475-82.
- Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, et al. Cancer treatment and survivorship statistics, 2019. 2019; 69: 363-85.
- Carrara S, Soldà G, Di Leo M, Rahal D, Peano C, Giunta M, et al. Side-by-side comparison of nextgeneration sequencing, cytology, and histology in diagnosing locally advanced pancreatic denocarcinoma. 2021; 93: 597-604. e5.
- Ilic M, Ilic IJWjog. Epidemiology of pancreatic cancer. 2016; 22(44): 9694.
- Yadav D, Lowenfels ABJG. The epidemiology of pancreatitis and pancreatic cancer. 2013; 144: 1252-61.
- Ge L, Pan B, Song F, Ma J, Zeraatkar D, Zhou J, et al. Comparing the diagnostic accuracy of five common tumour biomarkers and CA19-9 for pancreatic cancer: a protocol for a network meta-analysis of diagnostic test accuracy. 2017; 7: e018175.
- Rahib L, Wehner MR, Matrisian LM, Nead KTJJno. Estimated Projection of US Cancer Incidence and Death to 2040. 2021; 4: e214708-e.
- Fadhilah LNJJIKSH. Leukosit dan Kadar Bilirubin Total pada Ikterus Obstruktif yang Disebabkan oleh Tumor Pankreas. 2020; 9: 183-9.
- Matsumoto T, Okabe H, Yamashita Y-i, Yusa T, Itoyama R, Nakao Y, et al. Clinical role of fludeoxyglucose (18F) positron emission tomography/computed tomography (18 F-FDG PET/CT) in patients with pancreatic neuroendocrine tumors. 2019; 49: 21-6.
- Smith RA, Andrews KS, Brooks D, Fedewa SA, Manassaram-Baptiste D, Saslow D, et al. Cancer screening in the United States, 2018: a review of current American Cancer Society guidelines and current issues in cancer screening. 2018; 68: 297-316.
- Xiao AY, Tan ML, Wu LM, Asrani VM, Windsor JA, Yadav D, et al. Global incidence and mortality of pancreatic diseases: a systematic review, meta-analysis, and meta-regression of population-based cohort studies. 2016; 1: 45-55.
- Simoes PK, Olson SH, Saldia A, Kurtz RCJCco. Epidemiology of pancreatic adenocarcinoma. 2017; 6: 24.
- Yadav S, Sharma P, Zakalik DJAjoco. Comparison ofDemographics, Tumor Characteristics, and Survival Between Pancreatic Adenocarcinomas and Pancreatic Neuroendocrine Tumors. 2018; 41: 485-19.