Japanese Journal of Gastroenterology Research
Review Article - Open Access, Volume 2
Radical antegrade modular pancreatosplenectomy (RAMPS) in pancreatic surgery: A systematic review and meta analysis
Kongyuan Wei1#; Dan Duan2,3#; Yuanyuan Li2,3; Jinhui Tian2,3*
1Department of General, Visceral and Transplantation Surgery, University of Heidelberg, Heidelberg, Germany.
2School of Nursing, Evidence-Based Nursing Center, Lanzhou University, Gansu Lanzhou, China.
3Evidence Based Medicine Centre, Lanzhou University, Lanzhou, Gansu, China.
# Equal Contribution.
*Corresponding Author : Jinhui Tian
Evidence Based Medicine Centre, Lanzhou University,
Lanzhou, Gansu, China.
Email: tianjh@lzu.edu.cn
Received : Jul 01, 2022
Accepted : Jul 25, 2022
Published : Aug 01, 2022
Archived : www.jjgastro.com
Copyright : © Tian J (2022).
Abstract
Introduction: Radical Antegrade Modular Pancreatosplenectomy (RAMPS) is regarded as the modified approach of Conventional Distal Pancreatectomy (CDP) and has been applied in left-sided pancreatic cancer worldwide, but it is still controversial if RAMPS is more beneficial for patients, especially for the oncological outcomes.
Materials and methods: Studies were sought systematically in MEDLINE, Web of Science and CENTRAL. The primary outcomes were R0 resection rate, lymph-node retrieval numbers, overall complications and overall survival rate. The secondary measures were operative time, length of postoperative hospital stay and intraoperative blood loss. Pooled results are presented as odds ratios (OR) or mean difference (MD) with 95% confidence interval (CI).
Results: Totally 9 observational studies with a total of 958 patients were included in the final analysis. The meta-analysis demonstrated that RAMPS had more lymph-node retrieval numbers (MD, 4.82, 95%CI (1.81~7.83); P=0.002), shorter postoperative hospital stay (MD, -4.97, 95%CI (-9.70~-0.25); P=0.04) and decreased intraoperative blood loss (MD, -185.63, 95%CI (-212.41~-158.85); P<0.001) compared to CDP. There were no significant differences between the two groups with respect to operative time (MD, -5.44, 95%CI (-52.58~-41.69); p>0.05), R0 resection rate (OR, 1.55, 95% CI, (0.78 ~ 3.10); p>0.05), overall complications (OR, 0.66, 95%CI (0.23~1.87); p>0.05), overall survival rate (OR, 1.30, 95%CI (0.46~3.69); p>0.05).
Conclusions: This meta-analysis indicates that RAMPS is superior to CDP in terms of better oncological outcomes with less intraoperative blood loss and shorter postoperative hospital stay. Further evidence will be needed to verify the results.
Keywords: Radical antegrade modular pancreatosplenectomy (RAMPS); Conventional distal pancreatectomy; Meta analysis.
Citation: Wei K, Duan D, Li Y, Tian J. Radical Antegrade Modular Pancreatosplenectomy (RAMPS) In Pancreatic Surgery: A Systematic Review and Meta Analysis. Japanese J Gastroenterol Res. 2022; 2(11): 1100.
Introduction
Pancreatic cancer is one lethal tumor in gastrointestinal disease and becoming the second leading death carcinoma in next decades with a with a 5-year overall survival (OS) rate nearly 10% [1,2]. Surgery remains the most curative method for treating pancreatic tumors [3]. Conventional Distal Pancreatectomy (CDP) was reported for the left-sided pancreatic cancer but had unsatisfactory results with a 5-year overall survival of 6-30% [4,5]. Whereas CDP has some limitations in leading to improved clinical outcomes, the surgical research has not been stopped. From 2003, Radical antegrade modular pancreatosplenectomy (RAMPS) was introduced as one novel approach of the modified CDP [6].
RAMPS was regarded to make up part disadvantages of CDP and provide a better surgical vision through providing a posterior dissection plane [7]. After the wide application of RAMPS, this method attains the possibility to reduce the positive margin resection and increase the lymph node retrieval and R0 rates by systematic review and meta analysis [8-10]. Actually, CDP is always considered as the standard surgery for left-sided pancreatic cancer in spite of some unsatisfactory oncological outcomes which may influence the patients’ long-term quality of life (QOL). Pervious systematic review indicated that RAMPS is safe and feasible compared to DP, but due to the included sample size is not enough, the level of evidence should be improved with more included studies [8,10]. This updated systematic review and meta analysis aims to confirm the superiority of RAMPS in contrast to CDP scientifically and prudently.
Method
Literature search strategies
A systematic literature retrieval of relevant studies was performed up to September 2021 in PubMed, Embase, the Cochrane Library and Web of Science. The following key words were used to search related studies: “radical antegrade modular pancreatosplenectomy” or “RAMPS”. The authors also performed a search of the reference list of selected articles.
Inclusion and exclusion criteria
Two reviewers (KY W and DD) independently selected eligible article according to the predefined criteria. Discrepancies were resolved by discussions with a third reviewer (JH T). Inclusion criteria were: (1) literature design type: clinical trials or observational studies (including cohort and case-control studies); (2) the included patients were clearly diagnosed; (3) included items in the study for comparison: R0 resection rates (R0 resection indicates a microscopically margin-negative resection, in which no gross or microscopic tumor remains in the primary tumor bed), lymph-node retrieval, overall complications, overall survival, etc. should be available; (4) the studies focused on the RAMPS vs CDP and (5) language of the included study is limited to English. Exclusion criteria were: (1) abstracts, letters and case reports, etc; (2) literatures that were not comparative or not related to RAMPS procedure or CDP; (3) articles not reporting the assessmet of the beneficial effects or harms of the treatments (postoperative outcomes or HR and 95%CI); and (4) studies with data duplication.
Quality assessment
Two separate authors (KY W and DD) assessed the quality of included studies. The quality of included studies were assessed using the Newcastle-Ottawa Scale (NOS) for each included articles. Included literatures were ranked with a maximum of 9 points, including three parts: “selection”(four elements) “comparability”(one element) and “outcome”(three elements). Included studies with a NOS score <6 were considered of moderate or low quality [11]. As for the randomized controlled trials (RCTs), the Jadad scale was applied to evaluate the quality of the articles. Jadad score more than 4 was regarded as moderate or high quality.
Literature screening and data extraction
Literature screening: two researchers (KY W and DD) independently excluded the articles that clearly did not meet the inclusion criteria through reading the title and abstract of the included literatures. Then reading the full text of the studies that seemed to meet the inclusion criteria to select the study which met the inclusion criteria precisely. If there were discrepancies during the screening process, a resolution was available through discussion with a third reviewer (JH T).
Data extraction: The extracted data included study characteristics (title, authors, publication date, study period), patient characteristics (age, sex, body mass index, etc), number of cases, outcome measures between RAMPS and CDP, such as R0 resection rates, lymph-node retrieval, overall complications, overall survival, etc. For the outcomes of interest, when continuous variable were reported only as medians and ranges, the methods were applied to calculate means and standard deviations. The protocol of this study has been registered in PROSPERO: CRD42021249100.
Statistical analysis
All statistical analyses in the study were performed using Review Manager 5.4 Software and Stata software version 12.0. For continuous outcomes, weighted mean differences (MD) and corresponding 95% confidence intervals (CI) were calculated by the inverse variance method. For dichotomous outcomes, odds ratios (OR) and the corresponding 95% CI were calculated using the Mantel-Haenszel (MH) method. For the assessment of statistical heterogeneity, the I² statistic was used. If I² is greater than 50% statistical heterogeneity was considered to be high [12]. Due to the clinical heterogeneity and for a relatively conservative perspective, a random-effects model had been chosen for the meta-analyses regardless of the presence or absence of statistical heterogeneity. Potential publication bias for the primary outcomes were assessed using funnel plot and the regression test. A value of P<0.05 was considered to be statistically significant, and the 95% (CI) was set for effect measures.
Results
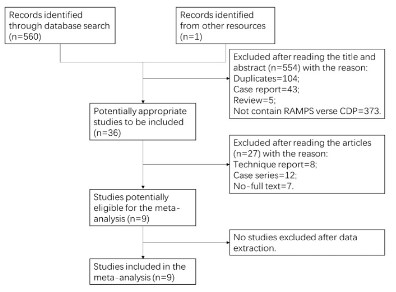
The flowchart of the literature selection process is shown in figure 1. Of 560 studies identified, we carefully evaluated the full text of 17 articles. Finally, nine studies (6 case-control studies [14-17,20,21] and 3 cohort studies [13,18,19] met all of the inclusion for the meta-analysis. The detailed characteristics and quality of the included studies are described in table 1. No RCTs had been published at the time of our search. The Newcastle Ottawa scale was used to evaluated the risk of bias. All included studies earned a score of 7 or more and were considered high quality (Additional file 1: Table S1).
Table 1: Characteristics of included studies.
| References | Country | Published Year | Group | No. of patients | Age (year) | M/F | BMI (kg/m2) | Tumor size (cm) | CA19–9 level (U/ml) | Well-moderate differentiation | Quality of studya | Dai M [3] | China | 2021 | RAMPS | 46 | 62.04 ± 8.83 | 23/23 | 22.94 ± 2.90 | 4.31 ± 1.99 | NA | 34 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| CDPS | 57 | 62.16 ± 10.24 | 28/29 | 23.90 ± 3.33 | 4.19 ± 1.76 | NA | 39 | ||||
| Kim HS [4] | Korea | 2021 | RAMPS | 37 | 67.27 ± 9.29 | 13/24 | NA | 3.79 ± 1.43 | 249.3 | 33 | 7 | CDP | 37 | 64.30 ± 10.79 | 21/16 | NA | 3.95 ± 2.27 | 212.76 | 32 |
| Kim EY [5] | Korea | 2016 | RAMPS | 30 | 63.7 ± 8.2 | 13/17 | 22.5 ± 3.3 | 4.6 ± 1.6 | NA | NA | 8 |
| DP | 19 | 62.1 ± 8.5 | 7/12 | 22.6 ± 2.7 | 4.5 ± 1.5 | NA | NA | ||||
| Abe T [6] | Japan | 2016 | RAMPS | 53 | 68.6 ± 10.7 | 31/22 | NA | NA | 136.4±291.0 | NA | 7 |
| SRPS | 40 | 65.2 ± 8.6 | 29/11 | NA | NA | 390.4±1157.1 | NA | ||||
| Trottman P [7] | USA | 2014 | RAMPS | 6 | NA | NA | NA | NA | NA | NA | 8 |
| standard resection | 20 | NA | NA | NA | NA | NA | NA | ||||
| Lee SH [8] | Korea | 2014 | RAMPS | 10 | 63.3 ± 9.9 | 6/4 | 24.2 ± 3.5 | 2.3 ± 0.6 | NA | 10 | 9 |
| open DPS | 40 | 62.7 ± 9.1 | 25/15 | 23.2 ± 2.8 | 3.2 ± 1.5 | NA | 33 | ||||
| Sham JG [9] | China | 2020 | RAMPS | 253 | 55 | 151/102 | NA | 4.8 (3.3-56) | NA | 10 | |
| CDP | 193 | 69 | 100/93 | NA | 3.9 (3.0-5.2) | NA | NA | ||||
| Park HJ [10] | Korea | 2014 | RAMPS | 38 | 62.17 (40–75) | 23/15 | NA | 3.1 (2–8.0) | NA | NA | 8 |
| CDPS | 54 | 61.25 (37–79) | 35/19 | NA | 3.8 (1–11) | NA | NA | ||||
| Latorre M [11] | Italy | 2013 | RAMPS | 8 | 61 | 5/3 | NA | NA | NA | NA | 8 |
| SPS | 17 | 60 | 11/6 | NA | NA | NA | NA |
M/F: male/female; NA: not available; a: according to Newcastle-Ottawa quality assessment scale
Characteristics of included studies
We included 9 articles [13-21] in the meta-analysis involving 958 participants. Four of the nine studies were conducted in Korea [14,15,18,20], two in China [13,19], one in Japan [16], one in USA [17] and one in Italy [21]. The range of the sample size was from 25 to 446 participants (median sample 106 people). The range of the participants’ age was from 37 to 80 years old (median age 58.50 years old). The number of male in the total included study population were 521. Only three studies [13,15,18] referred to the BMI, the range of the BMI was 19.2 to 27.7 kg/m2 (median BMI 23.22 kg/m2). And the CA19-9 was mentioned only by 3 articles [13,14,16]. One [16] article referred to the Initial CEA, one [13] referred to the Albumin and three [13,16,18] referred to additional therapy. There were no significant differences in these demographic characteristics. The allocation bias in all literatures for patients who underwent RAMPS or CDP may have influenced outcomes. Furthermore, four studies mentioned the follow-up, but all of the studies were unclear about the follow-up method.
Data analysis
Main outcome
R0 resection rate: Seven of the included studies reported R0 resection rate (13-16,18-20). 901 patients were involved in the studies. The R0 resection rate was 87.90% (407/463) in the RAMPS group and 85.39% (374/438) in the CDP group. The overall analysis revealed that there was no significant difference between the RAMPS group and the CDP group [OR 95% CI, 1.55 (0.78 ~ 3.10); P = 0.21] (Figure 2a). Heterogeneity was detected (P=0.03, I2 =57%), and the random-effects model was used.
lymph-node retrieval
The seven studies reported lymph-node retrieval numbers [13-18,21]. The studies covered 414 patients to make comparison in the number of lymph-node retrieval. Overall analysis revealed that the number of lymph-node retrieval was significantly higher in the RAMPS group than in the CDP group [MD 95%CI, 4.82(1.81~7.83); P=0.002] (Figure 2b). Heterogeneity was detected (P=0.007, I2 =66%), and the random-effects model was used.
Overall complications
Six studies reported overall complications rate involving 767 patients [13,15-19]. No significant difference was found when comparing RAMPS (29.15%, 116/398) with CDP (52.03%, 192/369) [OR 95%CI, 0.66(0.23~1.87); P=0.43] using a randomeffect model (P<0.001, I2 =85%) (Figure 2c).
Overall survival
294 patients were involved in four included studies reported the overall survival rate [13,14,20,21]. Heterogeneity was detected (P=0.03, I2 =68%), and the random-effects model was used. The overall survival rate was 27.13% (35/129) in the RAMPS group and 20.61% (34/165) in the CDP group. Overall analysis revealed no significant difference between RAMPS and CDP [OR 95%CI, 1.30(0.46~3.69); P=0.62] (Figure 2d).
Additional outcome
Meta-analysis results for additional outcome, including operative time (the time between start of the surgery (incision) and the finish of surgery (closure of the skin)), length of postoperative hospital stay (the time from the last operation until discharge) and blood loss are summarized in Table 2. Postoperative stay in the RAMPS group was significantly lower than that in the CDP group[MD 95%CI, -4.97(-9.70~-0.25); P=0.04] without increased intraoperative blood loss [MD 95%CI, -185.63(- 212.41~-158.85); P<0.001]. We found no statistically significant difference between RAMPS and CDP as regards the operative time (Additional file 2: Figure S1, Additional file 3: Figure S2, Additional file 4: Figure S3).
Table 2: Additional results of meta-analysis for RAMPS verse CDP.
| Outcome | Ref. included | No. of patients with RAMPS vs CDP | Heterogeneity Chi-square test | Model used | Mean difference | 95% CI | P value |
|---|---|---|---|---|---|---|---|
| Operative time (min) | [13-18] | 182 vs 213 | P < 0.01; I2= 94% | Random effect | -5.44 | -52.58~-41.69 | 0.82 |
| Hospital stay (days) | [13-18] | 182 vs 213 | P < 0.01; I2= 90% | Random effect | -4.97 | -9.70~-0.25 | 0.04 |
| Blood loss (ml) | [13-18] | 182 vs 213 | P < 0.01; I2= 73% | Random effect | -185.63 | -212.41~-158.85 | 0.01 |
CI: confidence intervals.
Sensitivity analyses
To test the stability of the overall meta-analysis results, sensitivity analyses were conducted by Stata software (Additional file 5: Figure S4; Additional file 6: Figure S5). Then excluding studies with the small cases to perform sensitivity analyses [15,17,18,21]. The results of these analyses revealed no significant differences when compared with the former estimates (Additional file 7: Table S2).
Publication bias
Egger’s test for lymph-node retrieval (t=-1.12, p=0.381), R0 resection rates (t=2.07, p=0.093), overall complications (t=2.61, p=0.059) and overall survival (t=-0.83, p=0.495) revealed no publication bias.
Discussion
In this study, 9 clinical trials with 958 participants were included and analyzed. Finally, RAMPS demonstrated the superior clinical outcomes compared to CDP with less intraoperative blood loss, shorter hospital of stay and higher number of lymph-node retrieval. As for the operative time, R0 resection rate, overall complications and overall survival, RAMPS showed no significant difference in comparison with CDP. But in terms of advantages of RAMPS, the results of the intraoperative blood loss, hospital of stay and number of lymph-node retrieval held moderate to high heterogeneity, after performing the sensitivity analysis and publication bias analysis, the evidence of these results are convincible.
Given the results of previous meta analysis, RAMPS was proved to attain higher R0 resection rate and harvest of more lymph nodes with 378 patients in contrast to standard procedure in the treatment of left-sided pancreatic cancer [8] while in our study, R0 resection rate is not obviously different in both groups. Another meta analysis with total 285 patients reported that there were significant difference among operation time, bleeding volume, R0 resection rate, number of lymph node excision and one-year overall survival between RAMPS and DP [10]. Considering the diversity of the results, the sample size is one important factor affecting the evidence and the risk of bias also contributed to the difference. However, it can be at least verified that RAMPS implied the benefit for the patients with pancreatic cancer.
From the results of our study, RAMPS has the potential to reduce the intraoperative blood loss. It is possibly because that RAMPS provides a more clearer surgical vision for surgeons to perform the resection conveniently. The posterior dissection plane allows the improvement of surgical skills to be carried out. Although there was no statistical significance in overall complications in both groups, the shorter length of hospital stay indirectly displayed that patients with RAMPS perhaps achieve a fast recovery after operation to some extent. Further evidence is needed to verify the results.
Unlike the CDP, the antegrade approach make it easier for surgeon to control the splenic vein, adrenal vein, and renal vein during the operation. Additionally, RAMPS pays more attention to the negative margin resections and complete N1 node dissections, in accordance with the results of our study, RAMPS truly had more number of lymph-node retrieval. The modification of the CDP provides a novel concept of radical pancreatic resection for left-sided pancreatic cancer whereas there is limited RCT focusing on the long-term overall survival of RAMPS.
Compared to the conventional distal pancreatectomy, RAMPS displayed no obvious difference in R0 resection rate, overall complications, overall survival and operation time. In detail, for R0 resection rate, only Abe’s study showed that RAMPS had high R0 resection rate while the rest studies did not imply significant difference in both groups. Sham’s study reported that RAMPS attained less overall complications and the others showed no difference between RAMPS and CDP. Additionally, Park’s study implied better overall survival in contrast to CDP with no distinct difference among other studies. Abe’ study proved that RAMPS achieved shorter operation time. Although there were no evident difference in total effect in terms of R0 resection rate, overall complications, overall survival and operation time, several studies mentioned above truly showed the advantages of RAMPS compared to CDP respectively. Hence, we may postulate that RAMPS has the potential to be superior to CDP regard to improving the QOL of patients in the future. To investigate the real reason for the benefit of RAMPS, there are some theoretical findings: RAMPS hold the ability to provide the advanced visualization of the posterior plane of dissection, proper vascular control in advance and negative tangential margin rates [22,23]. Further researches are needed to confirmed the hypothesis.
However, this study has some limitations as follows: 1. there is no RCT among all the included studies possibly leading to the bias, although NOS score was used to evaluate the quality of included studies; 2. during conducting this meta-analysis, some included studies did not have the standard definition for some index such as LOH, operation time resulting in some bias in the calculation; 3. the sample size of this study may be not big enough to produce more scientific and prudent evidence as designed before.
Conclusion
In summary, RAMPS is beneficial for patients with less intraoperative blood loss, shorter postoperative hospital stay and more lymph-node retrieval number compared to CDP. RAMPS can be the optimal method for patients with left-sided pancreatic cancer.
Declaration
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Authors’ contributions: KYW, DD, YYL and JHT designed the study. KYW drafted the protocol, with assistance from DD. YYL will perform the literature search. KYW and DD will carry out the data collection and YYL will assist with data collection as the third reviewer. KYW, DD and YYL will perform quality assessment. KYW will complete the data analysis with statistical assistance from DD and YYL. KYW, DD and YYL will draft the final manuscript, which will be reviewed by all co-authors. JHT will be the guarantor of the review. All authors gave final approval of the version to be published and agreed to be accountable for all aspects of this work.
References
- Grossberg AJ, Chu LC, Deig CR, et al. Multidisciplinary standards of care and recent progress in pancreatic ductal adenocarcinoma. CA Cancer J Clin. 2020; 70: 375-403.
- Strobel O, Neoptolemos J, Dirk Jäger D, et al. Optimizing the outcomes of pancreatic cancer surgery. Nat Rev Clin Oncol. 2019; 16: 11-26.
- Hackert T, Klaiber U, Pausch T, et al. Fifty Years of Surgery for Pancreatic Cancer. Pancreas. 2020; 49: 1005-1013.
- Wu X, Tao R, Lei R, et al. Distal pancreatectomy combined with celiac axis resection in treatment of carcinoma of the body/tail of the pancreas: a single-center experience. Ann Surg Oncol. 2010; 17: 1359–66
- Yamamoto J, Saiura A, Koga R, et al. Improved survival of leftsided pancreas cancer after surgery. Jpn J Clin Oncol. 2010; 40: 530–6.
- Strasberg SM, Drebin JA, Linehan D. Radical antegrade modular pancreatosplenectomy. Surgery. 2003; 133: 521-7.
- Dragomir M, Eftimie MA. Is Radical Antegrade Modular Pancreatosplenectomy the Solution? A Systematic Literature Review and Meta-Analysis. Chirurgia (Bucur). Nov-Dec 2017; 112: 653- 663.
- Cao F, Li J, Li A, et al. Radical antegrade modular pancreatosplenectomy versus standard procedure in the treatment of left-sided pancreatic cancer: a systemic review and meta-analysis. BMC Surg. 2017; 17: 67.
- Huo Z, Zhai S, Wang Y, et al. Comparison of radical antegrade pancreatosplenectomy with standard retrograde pancreatosplenectomy for left-sided pancreatic cancer: a meta-analysis and experience of a single center. Med Sci Monit. 2019; 25: 4590-460.
- Zhou Q, Gao F, Gong J, et al. Assessment of postoperative longterm survival quality and complications associated with radical antegrade modular pancreatosplenectomy and distal pancreatectomy: A meta-analysis and systematic review. BMC Surg. 2019; 19: 12.
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010; 25: 603-5.
- Higgins JP, Thompson SG. Quantifying heterogeneity in a metaanalysis. Stat Med. 2002; 21: 1539-58.
- Dai M, Zhang H, Li Y, et al. Radical antegrade modular pancreatosplenectomy (RAMPS) versus conventional distal pancreatosplenectomy (CDPS) for left-sided pancreatic ductal adenocarcinoma. Surg Today. 2021; 51: 1126-1134.
- Kim HS, Hong TH, You YK, et al. Radical antegrade modular pancreatosplenectomy (RAMPS) versus conventional distal pancreatectomy for left-sided pancreatic cancer: findings of a multicenter, retrospective, propensity score matching study. Surg Today. 2021.
- Kim EY, You YK, Kim DG, et al. Initial experience with radical antegrade modular pancreatosplenectomy in a single institution. Ann Surg Treat Res. 2016; 91: 29-36.
- Abe T, Ohuchida K, Miyasaka Y, et al. Comparison of Surgical Outcomes Between Radical Antegrade Modular Pancreatosplenectomy (RAMPS) and Standard Retrograde Pancreatosplenectomy (SPRS) for Left-Sided Pancreatic Cancer. World J Surg. 2016; 40: 2267-75.
- Trottman P, Swett K, Shen P, et al. Comparison of standard distal pancreatectomy and splenectomy with radical antegrade modular pancreatosplenectomy. Am Surg. 2014; 80: 295-300.
- Lee SH, Kang CM, Hwang HK, et al. Minimally invasive RAMPS in well-selected left-sided pancreatic cancer within Yonsei criteria: long-term (>median 3 years) oncologic outcomes. Surg Endosc. 2014; 28: 2848-55.
- Sham JG, Guo S, Ding D, et al. Radical antegrade modular pancreatosplenectomy versus standard distal pancreatosplenectomy for pancreatic cancer, a dual-institutional analysis. Chin Clin Oncol. 2020; 9: 54.
- Park HJ, You DD, Choi DW, et al. Role of radical antegrade modular pancreatosplenectomy for adenocarcinoma of the body and tail of the pancreas. World J Surg. 2014; 38: 186-93.
- Latorre M, Ziparo V, Nigri G, et al. Standard retrograde pancreatosplenectomy versus radical antegrade modular pancreatosplenectomy for body and tail pancreatic adenocarcinoma. Am Surg. 2013; 79: 1154-8.
- Chun YS. Role of Radical Antegrade Modular Pancreatosplenectomy (RAMPS) and Pancreatic Cancer. Ann Surg Oncol. 2018; 25: 46-50.
- Strasberg SM, Fields R. Left-sided pancreatic cancer: distal pancreatectomy and its variants: radical antegrade modular pancreatosplenectomy and distal pancreatectomy with celiac axis resection. Cancer J. Nov-Dec 2012; 18: 562-70.