Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 2
Gastric cancer complicated with primary liver cancer: A case report
Yan Chen1*; Ping Wang2; Ying-Jian Zhang1*
1Department of Gastroenterology, The First Affiliated Hospital, and College of Clinical Medicine of Henan University of Science and Technology, Luoyang 471003, Henan, China.
2Department of Public Health, School of Medicine, Henan University of Science and Technology, Luoyang 471003, Henan, China.
*Corresponding Author : Yan Chen & Ying-Jian Zhang
Department of Gastroenterology, The First Affiliated
Hospital, and College of Clinical Medicine of Henan
University of Science and Technology, No. 24 Jinghua
Road, Luoyang 471003, Henan, China.
Tel: +86-379-69823576 & 13783131268;
Email: cy15036625181@163.com
Received : Jun 10, 2022
Accepted : Jul 05, 2022
Published : Jul 12, 2022
Archived : www.jjgastro.com
Copyright : © Chen Y & Zhang YJ (2022).
Abstract
Multiple primary cancer (MPC) is caused by a variety of factors such as genetic factors, living environment factors, iatrogenic factors and so on. According to the difference in the interval between the two cancers, it can be divided into simultaneous MPC and heterochronous MPC. Due to the large individual difference of MPC patients, the diagnosis and treatment process of MPC is relatively complicated. At present, the clinical understanding of MPC is still insufficient, and there is still no unified standard for the treatment of MPC. Clinicians pay insufficient attention to multiple primary cancers, or are easily confused with metastasis and recurrence of multiple primary cancers, resulting in misdiagnosis and missed diagnosis, resulting in patients losing the best opportunity for treatment. The treatment and prognosis of MPC are completely different from those of metastatic and recurrent cancers, which shorten the survival period of patients. Therefore, attention should be paid to the study of multiple primary cancers. We report a case of gastric cancer complicated with primary liver cancer admitted to the First Affiliated Hospital of Henan University of Science and Technology.
Keywords: MPC; Gastric cancer; Liver cancer; Heterochronous; PLC.
Citation: Chen Y, Wang P, Zhang YJ. Gastric cancer complicated with primary liver cancer: A case report. Japanese J Gastroenterol Res. 2022; 2(10): 1096.
Case report
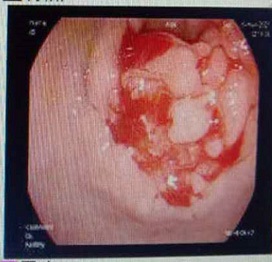
The patient, a 55-year-old male, was admitted to the hospital on March 11, 2021 due to “upper abdominal distension, pain and discomfort for more than 1 year, and recurrence for more than 2 months”. More than 1 year ago, the patient had no obvious inducement of upper abdominal distension, pain and discomfort, no acid reflux, heartburn, no nausea, vomiting, no hemesis, melena, no chest pain, chest tightness and other discomfort, no care, no diagnosis and treatment. Before 2 months, the patient’s symptoms were aggravated again, and the symptoms continued to be not relieved, so the emergency department was admitted to our hospital as “abdominal distension cause check”. Previous healthy, smoking and drinking history, no similar patients in the family. Improve relevant examinations after admission, such as: Infectious disease screening: hepatitis B surface antigen (gold standard method) positive (+), HBVDNA: 3.89 x 106 IU/ml, TAP: 128.03 um², liver function:TP: 50.23 g/L ALB: 27.8 g/L, TBIL: 34.8 g/L, DBIL: 15.00 g/L, IBIL: 19.8 g/L, ALT: 27 g/L, AST: 51 g/L, PCHE: 1879 g/L, AFP: 203.8 ng/ml, Color Doppler ultrasonography of chest and abdomen showed that liver cirrhosis was possible, portal vein velocity decreased, liver disease gallbladder, splenomegaly and splenic vein dilation. 256 row chest and upper abdomen CT (plain scan + enhanced): 1. Ground glass shadow of left lung, follow-up and reexamination are recommended; 2. Liver cirrhosis, splenomegaly, esophagogastric fundus and splenic collateral circulation; The abnormal enhancement focus in the right lobe of the liver, considering the high possibility of liver cancer, the remaining small nodule like enhancement in the liver, considering intrahepatic metastasis (Figure 1). 3. Gastric antrum space occupying, considering malignancy, please combine clinical and pathological findings. 3.0 Mr upper abdomen (plain scan + enhancement): 1. Liver cirrhosis with regenerative nodules, splenomegaly, portal hypertension, ascites and collateral circulation; 2. Abnormal signal of right posterior lobe of liver (Figure 2). Considering malignancy, please combine clinical and AFP examination. Gastroscopy showed: 1. Esophageal gastric fundus varices (severe); 2. Gastric antrum space occupying: Ca? (Figure 3); Gastric antrum pathology (HE staining Figure 4) results: (gastric antrum) adenocarcinoma. Liver puncture pathology (immunohistochemical (Figure 5) diagnosis: (liver puncture) combined with immunohistochemical results, it is consistent with hepatocellular carcinoma. Immunohistochemistry: CerbB2 (0), CK (+), HEPA (partial +), glypican (+), CD (small amount +), CD34 (blood sinus +), CK7 (-), CK8 (+), CK19 (-), CDX2 (-), Ki67 (50% +), GS (+), CK20 (-). Physical examination: Body temperature was 37OC, pulse was 78 beats/ min, respiration was 20 beats/min, blood pressure was 120/70 MHg, skin and mucosa of the whole body were mildly yellow, no rash, bleeding spots, liver palm or spider nevus, superficial lymph nodes were not touched and enlarged, and no obvious abnormalities were found in head, neck, heart and lungs during physical examination. Abdominal distention, soft abdomen, no obvious tenderness, rebound pain and muscle tension in the abdomen, liver, spleen and ribs are not touched, negative mobility dullness, bowel sounds are normal. The patient refused interventional therapy, asked for oral chemotherapy and was discharged after her symptoms improved.
Discussion
Multiple primary carcinoma (MPC) is defined as the simultaneous or continuous occurrence of more than two types of primary malignant tumors in a single organ or different organs in the same individual. MPC is often occult, with atypical clinical symptoms and heterogeneous cancer manifestations, which can be confused with primary cancer metastasis, so it is easy to be ignored clinically. This article reviewed the clinical characteristics of a patient with gastric cancer complicated with primary liver cancer admitted to the Department of Gastroenterology, The First Affiliated Hospital of Henan University of Science and Technology, aiming to arouse clinicians' attention to multiple primary cancers and improve the diagnosis rate of multiple primary cancers.
Gastric cancer, as one of the most common malignant tumors of digestive tract, has a high incidence in China and is reported to rank first in the incidence of malignant tumors [1]. There are no obvious symptoms or manifestations of gastric cancer in the early stage, and it is often in the middle and late stage when it is diagnosed, so the best treatment opportunity has been missed, and the life safety of patients will be severely threatened [2]. Gastric cancer is a malignant tumor originating from gastric mucosa, which is closely related to Helicobacter pylori (Hp). In 1994, WHO listed Helicobacter pylori as a class i carcinogen. China is a region with a high incidence of gastric cancer, and its morbidity and mortality are far higher than the world's average level. It is a major public health problem that needs to be addressed urgently. The incidence of gastric cancer in China is widely distributed with obvious differences, especially in the northwestern and southeastern coastal areas [3]. The incidence of gastric cancer increases gradually with the increase of age, and the peak age of incidence is 40-60 years old, and the incidence of male is about twice that of female [4]. Primary hepatic carcinoma (PLC) is the fifth largest cancer in the world and the third leading cause of cancer-related death. As a result, it has become a major public health problem that endangers people's life and health Carcinoma, HCC) accounted for more than 90%. Chronic hepatitis B virus (HBV) infection accounts for most of the risk factors leading to HCC. Epidemiological studies have shown that hepatitis B virus X (HBx) is the core functional protein of HBV and plays an important role in the development of HBV-HCC. This patient has a history of HEPATITIS B.
Multiple primary carcinoma, also known as repeated carcinoma and multiple carcinoma, is a rare phenomenon in oncogenesis. With the diversification of malignant tumor treatment means, the survival time of patients is prolonged, especially in the aging society, because the elderly are also a high-risk group prone to multiple primary cancers, and the incidence rate is increasing [5]. At present, the diagnostic criteria proposed by Billroth and revised by Warran are mostly adopted : ① Each tumor must be malignant. ② Each tumor exists independently of each other. ③ There must be a certain distance of normal tissue between the carcinomas. ④ A tumor must be excluded as a metastasis to other tumors. Most of the multiple primary cancers are easy to diagnose, but the invasion and metastasis of the first cancer should be excluded according to the pathological tissue image when determining the second primary cancer [6]. This case meets this criterion. Currently, most scholars cite Moertel's proposal that synchronous carcinoma (SC) is defined as multiple malignant tumors occurring within 6 months apart, and meTAC - Hronous carcinoma (METAC - Hronous carcinoma) is defined as multiple malignant tumors occurring within 6 months apart. MC. Combined with the patient's medical history and related examinations, this case belongs to simultaneous multiple primary carcinoma.
At present, the etiology and pathogenesis of multiple primary carcinoma remain unclear. Multiple primary cancers are more common in the elderly and may be related to the following factors: (1) Host susceptibility is related to oncogenes. Overexpression of oncogenes and loss and variation of tumor suppressor genes are significantly related to the occurrence of multiple primary cancers, especially in people with a family history of cancer [13]. The occurrence of multiple primary cancers usually involves gene variation. It may be associated with U1snRNA mutation [7], abnormal expression of circR NA and SNHG15 [8,9], CDH1 mutation and activation of WNT/β-catenin signal [10]. (2) Clinical retrospective studies have shown that the risk of MPC is related to the patient's age and disease incubation period [11]. (3) A study on multiple primary cancers of gastric cancer found that tobacco is an important risk factor [12], which may be consistent with Slaughter's field Cancerization theory: Gastrointestinal, lung and urinary system are the channels of food, gas and excreta respectively. They receive chronic stimulation from common carcinogenic factors in food and air. (4) The immune deficiency of the body, the body resistance and immunity of the elderly are reduced, and the primary cancer may also reduce the host's resistance to secondary cancer; (5) Surgery, radiotherapy, chemotherapy, etc., may further damage the immune function and have certain influence on the environment; (6) Adverse lifestyle and genetic factors increase the risk of multiple primary cancers. (7) Due to the improvement of diagnosis and treatment, the survival time of tumor patients is significantly prolonged, resulting in increased sensitivity of cancer factors and multiple diseases; The patient was a middle-aged male, 55 years old, with reduced body resistance and immunity, high incidence of carcinoma in situ, bad habits such as smoking and drinking, and hepatitis B.
Conclusion
In conclusion, adequate understanding should be given to multiple primary cancers, especially for middle-aged and elderly patients. If clinical symptoms cannot be explained by a single tumor, the existence of multiple primary cancers should be considered. PET/CT has been reported to be helpful in the diagnosis of multiple primary cancers [14]. Follow-up work should be strengthened for the susceptible population of multiple primary cancers. Early diagnosis and early treatment are very important to its curative effect and prognosis. Once the diagnosis is confirmed, radical surgery should be pursued to improve the survival rate. Since radiotherapy and chemotherapy are the inducing factors of multiple cancers, individualized treatment plans should be formulated to minimize the possibility of recurrence of new cancers on the basis of the maximum benefit of patients.
Declarations
Acknowledgements: Not applicable.
Funding: This study was supported by the Scientific Research Fund of Henan Provincial Science and Technology Department (No.182102310302).
Contributions: Conception and design: Y. Chen, P. Wang, Y. J. Zhang. Analysis and interpretation of data: Y. Chen, P. Wang, Y.J. Zhang. Drafting of the article: Y. Chen, Y.J. Zhang. Critical revision of the article for important intellectual content: Y. Chen.,P. Wang, and Y. J. Zhang. Final approval of the article: Y. Chen, P. Wang, and Y.J. Zhang. Statistical expertise: P. Wang: Y. Chen, Y. J. Zhang . Administrative, technical, or logistic support: Y. Chen, P. Wang. Collection and assembly of data: Y. Chen. Obtaining funding. Y.J. Zhang. Study supervision. Y.J. Zhang.
Ethics approval and consent to participate: This study was approved by the ethics committee of the first affiliated hospital, and college of clinical medicine of henan university of science and technology. Informed consent for patient was obtained prior to therapy and performed in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines.
Consent for publication: Not applicable.
Competing interests: The authors declare that they have no competing interests.
References
- Liu J, Yunpeng L. Progress and prospect of international clinical research on drugs for gastric cancer. Chin J gastroenterol. 2020; 23: 196-200.
- Li G, Jinbao Z, Qiyu S. Contrast ultrasonography combined with gastroscopy in the diagnosis of early gastric cancer J. Imaging research med appl. 2019; 3: 214-215.
- Chang M, Jiucong Z, Zhou Q, et al. Progress in epidemiology of gastric cancer. Journal of Gastroenterology and Hepatology. 2017; 26: 966-969.
- Wenbin Z, Wu H, Quancai C, et al. Research progress on risk factors of gastric cancer. Chinese Journal of practical internal medicine. 2014; 34: 415-420.
- Xuejuan D, Changhao C, Benyan Wu, et al. Clinical analysis of 119 cases of multiple primary malignant tumors of digestive system in the elderly. PLA medical journal. 2008; 33: 317-319.
- Jianguang Y, Xiaoxia L, Fanmin K. Analysis of clinical characteristics of multiple primary cancers. Modern oncology medicine. 2011; 12: 1672-4992.
- Shuai S, Suzuki H, Diaz-Navarro A, et al. The U1 spliceosomal RNA is recurrently mutated in multiple cancers Nature. 2019; 574: 712-716.
- Yin Y, Long J, He Q, et al. Emerging roles of circ RNA in formation and progression of cancer. J Cancer. 2019; 10: 5015.
- Tong J, Ma X, Yu H, et al. SNHG15: A promising cancer-related long noncoding RNA Cancer Manag Res. 2019; 11: 5961-5969.
- Hu MN, Lv W, Hu Y, et al. Synchronous multiple primary gastrointestinal cancers with CDH1 mutations: A case report. World J Clin Cases. 2019; 7: 1703-1710.
- Shah B, Kandel P, Khanal A, Second Primary Malignancies in Hepatocellular Cancer - A US Population-based Study. Anticancer es. 2016; 36: 3511-3514.
- Morais S, Antunes L, Bento MJ, et al. Risk and survival of third primary cancers in a population-based cohort of gastric cancer patients. Dig Liver Dis. 2019; 51: 584-588.
- Belev Nf, Samotyia Ee, Pikhut Pm, et al. Genetic-epide-miologic study of adenoma and cancer of the large intestine J. Ge-netika. 1999; 35: 516-523.
- Long Sun, Ying Wan, Qin Lin, et al. Multiple primary malignant tumors of upper gastrointestinal tract: a novel of 18 F - FDG PET/ CT. World J Gastroenterol. 2010; 16: 3964-3969.