Japanese Journal of Gastroenterology Research
Clinical Image - Open Access, Volume 2
Epigastric pain and difficulty swallowing in a haemodialysis patient
Ming Chun Hsieh1; Yuan-Hung Wang1,2; Ruei-Lin Wang1; Wen-Fang Chiang3,4; Hung-Jui Hsu5; Po-Jen Hsiao3,4,6*
1Department of Internal Medicine, Taoyuan Armed Forces General Hospital, Taoyuan 325, Taiwan.
2Division of Cardiology, Department of Internal Medicine, Taoyuan Armed Forces General Hospital, Taoyuan 325, Taiwan.
3Division of Nephrology, Department of Internal Medicine, Taoyuan Armed Forces General Hospital, Taoyuan 325, Taiwan
4Division of Nephrology, Department of Internal Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan.
5Division of Gastroenterology, Department of Internal Medicine, Taoyuan Armed Forces General Hospital, Taoyuan 325, Taiwan.
6Department of Life Sciences, National Central University, Taoyuan 320, Taiwan.
*Corresponding Author : Po-Jen Hsiao
Division of Nephrology, Department of Internal Medicine,
Taoyuan Armed Forces General Hospital, Taiwan No.168,
Zhongxing Rd., Longtan Dist., Taoyuan City 325, Taiwan.
Tel: 886-3-4799595, Fax: 886-3-4801625;
Email: a2005a660820@yahoo.com.tw &
doc10510@aftygh.gov.tw
Received : May 19, 2022
Accepted : Jun 08, 2022
Published : Jun 15, 2022
Archived : www.jjgastro.com
Copyright : © Po-Jen H (2022).
Keywords: Epigastric pain; Difficulty swallowing; Oesophageal Candidiasis; Candida albicans.
Citation: Hsieh MC, Yuan-Hung W, Ruei-Lin W, Wen-Fang C, Po-Jen H, et al. Epigastric pain and difficulty swallowing in a haemodialysis patient. Japanese J Gastroenterol Res. 2022; 2(8): 1088.
Clinical image description
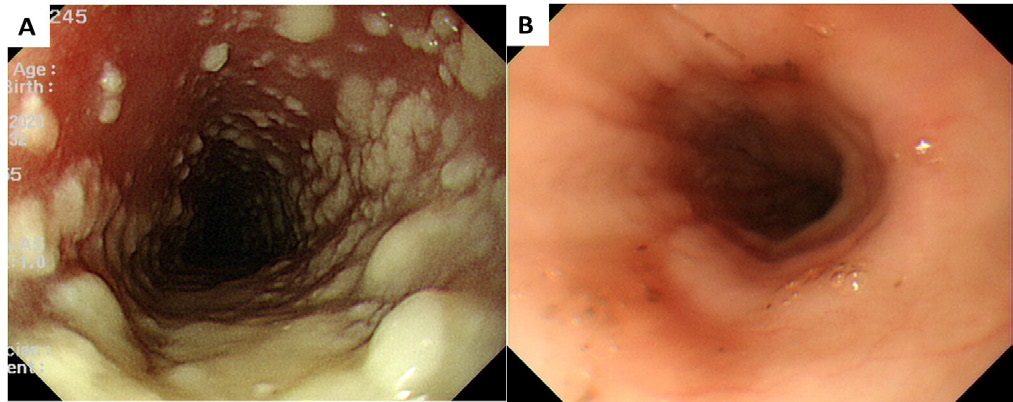
A 57-year-old man was admitted due to progressive epigastric pain and difficulty swallowing for 5 days. He had a history of type 2 diabetes mellitus and end-stage renal disease with regular haemodialysis maintenance. His family history was unremarkable. He had not received corticosteroids or other immunosuppressant medications. The patient had used proton pump inhibitors (20 mg/d omeprazole) for 2 months due to acid regurgitation. Oesophagogastroduodenoscopy revealed white, linear, mucosal, and plaque-like lesions on the oesophagus (Figure 1A). No oropharyngeal or gastroduodenal lesions were noted. The diagnosis of oesophageal candidiasis was made based on the typical endoscopic findings, which was confirmed by a pathology of oesophageal biopsy tissue that was positive for Candida albicans. A serologic test for human immunodeficiency virus was negative. Intravenous antifungal therapy was started in the patient, his epigastric pain was reduced within 1 week after initiated therapy. A follow-up endoscopy was performed 14 days after the initiation of antifungal therapy, which revealed an obvious improvement (Figure 1B).
The incidence of oesophageal candidiasis is 0.32% to 5.2% in the general population. The risk factors for oesophageal candidiasis include early or late age, use of proton pump inhibitors, smoking, an immunocompromised state and long-term treatment with antibiotics or corticosteroids [1,2]. Oesophageal candidiasis usually responds well to systemic antifungal therapy. Differential diagnoses, such as herpes simplex virus, cytomegalovirus, pill-induced oesophagitis, eosinophilic oesophagitis, radioactive oesophagitis, gastroesophageal reflux disease, and other types of oesophageal mucosa inflammation, should be considered in clinical practice [1-3].
Acknowledgements: We thank the patient’s consenting to publish the clinical information.
References
- Mohamed AA, Lu XL, Mounmin FA. Diagnosis and Treatment of Esophageal Candidiasis: Current Updates. Can J Gastroenterol Hepatol. 2019; 2019: 3585136.
- Kondo T, Terada K. Candida Esophagitis. N Engl J Med. 2017; 376: 1574.
- Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2016; 62: e1-e50.