Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 2
Rare pathogenic pulmonary infection in patients with ulcerative colitis: Case report
Fei Zhu1; Rui Huang1; Huifei Lian1; Liping Fang2; Gaofei Shen1; Xin Li1; Junyi Zheng1; Jinpeng Li1; Shuimiao Deng1; Baozhen Guo1; Zhenzhen Liu1*
1Gastrointestinal Endoscopy Center, Xi’an People’s Hospital (Xi’an Fourth Hospital), Xi’an 710000, China.
2Respiratory Chronic Diseases and Infectious Diseases Center, Xi’an People’s Hospital (Xi’an Fourth Hospital), Xi’an 710000, China.
*Corresponding Author : Zhenzhen Liu
Gastrointestinal Endoscopy Center, Xi’an People’s
Hospital(Xi’an Fourth Hospital), Xi’an 710000, China.
Email: liuzhen8080@163.com
Received : May 04, 2022
Accepted : Jun 01, 2022
Published : Jun 08, 2022
Archived : www.jjgastro.com
Copyright : © Liu Z (2022).
Abstract
In the treatment of Ulcerative Colitis (UC), the use of glucocorticoids, immunomodulators, and biologic therapies increases the risk of opportunistic infections. These Infections in patients with IBD include CMV and EB viruses, bacteria, Clostridium difficile, tuberculosi, fungal infections. We present a patient with severe UC after two induction and remission treatment with glucocorticoid and Infiximab (IFX), then the intestinal symptoms improved significantly, but in a short term appeared lung infection of Nocardia cyiacigeorigica and Pneumocystis jerovec (Pj). After combined anti-infection his condition improved significantly. This paper aims to warn clinicians to pay close attention to pulmonary opportunistic infections after the use of glucocorticoids and biologic agents in UC treatment.
Keywords: Ulcerative colitis; Opportunistic infection; Infliximab; Nocardia cyiacigeorigica; Pneumocystis jeroveci.
Citation: Zhu F, Huang R, Lian H, Fang L, Shen G, et al. Rare pathogenic pulmonary infection in patients with ulcerative colitis: Case report. Japanese J Gastroenterol Res. 2022; 2(8): 1087.
Introduction
For moderate to severe UC, the nutritional status of the patient is decreased due to the disease itself, and the application of glucocorticoids, immunosuppressants, biological agents significantly inhibit the immune system of the patient, prone to opportunistic infections. Multivariate analysis indicated that the use of any immunosuppressant yielded an OR of 3.247 (95% CI: 1.128-9.341), whereas the use of any two immunosuppressants yielded an OR of 6.457 (95% CI: 1.726-24.152) for opportunistic infection. When immunosuppressants were used in combination with Infliximab (IFX) or 5-aminosalicylic acid, a significantly increased risk of opportunistic infection was also observed [1,2].
Case report
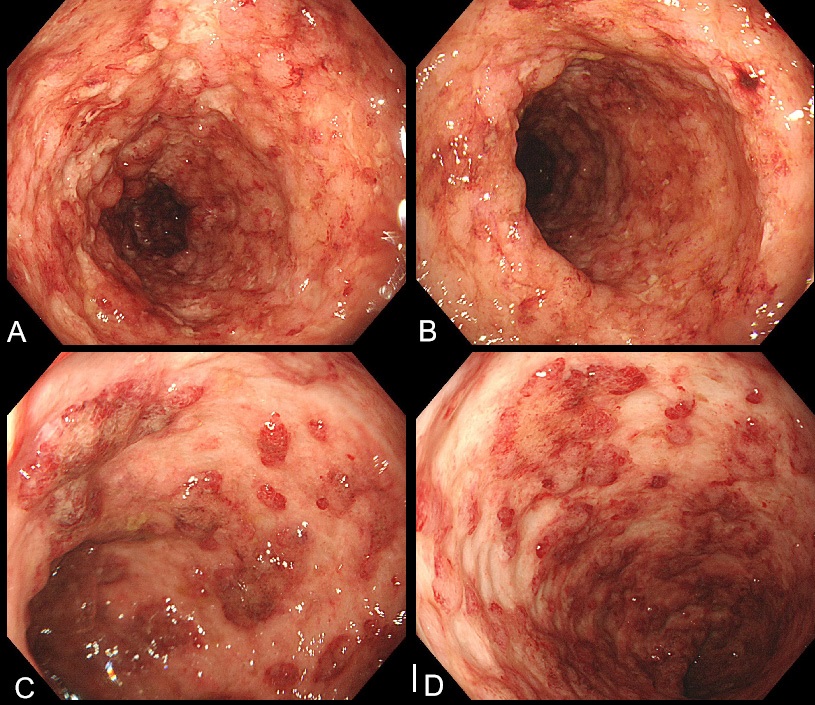
A 57-year-old man who was diagnosed with UC 3 years earlier was admitted to our hospital with abdominal pain and increased mucopurulent blood stool (more than 10 times/day) in August 2021. Laboratory tests showed increased Erythrocyte Sedimentation Rate (ESR, 23 mm/h)and low albumin (27.7 g/l). Autoantibody profile and a complete infectious workup turned out to be negative. Colonoscopy showed diffuse inflammation and ulcers in the left-sided colon (Figure 1). Chest Computed Tomography (CT) showed a small amount of pleural effusion, the initial consideration may be associated with hypoalbuminemia. We gived mesalazine 4 g/d and prednisone acetate (initial dose 35 mg/d), in addition considerd colonoscopy ulcer form cannot except with cytomegalovirus infection, empirical gived ganciclovir 250mg q12h. On 27 August and 8 September, He started induction therapy with infliximab 300 mg. Then the number of stools gradually decreased to 1-2 times / day.
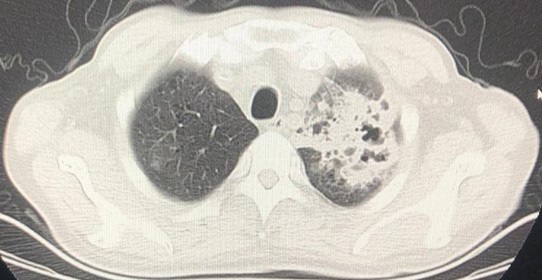
On September 23, he presented to our hospital again with high fever (up to 40°C) and cough. Laboratory tests showed elevated White Cell Count (WBC) of 20.03 X 109 /L neutrophil count of 14.08 X 109 /L and the procalcitonin of 0.86 ng/ml. Haemoglobin was decreased at 77 g/L. Both the fungal G and GM tests were negative. Multiple sputum smear showed a large number of G + cocci, a small amount of G-bacteria. Sputum culture indicated small growth of fungal bacteria. Analysis of blood gas: PH 7.45, PaO2 54.7 mmHg, PaCO2 40 mmHg, Oxygen saturation was 87.8%. Chest CT showed that double lung multiple dense density (Especially the left lung), a bilateral pleural effusion decreased compared with the anterior (Figure 2). Multiple sputum smears found a large number of G + cocci, a small number of Gbacilli, acid resistance stain negative. Pathogenic genetic testing of Bonchoalveolar Lavage Fluid (BALF) suggested that Nocardia cyiacigeorigica,and albicans Saccharomyces, Pneumocystis Jewel (PJ). For special infections in the lungs, we used Meropenem combined with linezolid compound, sulfamethoxazole to fight infection. For the UC, prednisone was continued and thalidomide was added the third IFX infusion was suspended. Then the patient's body temperature was normal, the inflammatory index dropped to normal.
Discussion
Common opportunistic infections in UC patients include CMV and EB viruses, Streptococcus pneumonia [1], fungus [2]. In this case, this patient quickly developed an opportunistic pulmonary infection after more than 1 month of glucocorticoid treatment and two times of IFX treatment. The results of BALF gene test suggested that the pathogenic bacteria were Nocardia cyiacigeorigica, albicans Saccharomyces, Pneumocystis jewel, which were very rare in UC patients. Nocardia cyiacigeorigica was discovered and redefined in Germany in 2001 by Yassin [3], relatively rare in domestic reports. Laboratory examination and Chest CT lack of specific changes, easy to misdiagnosis and miss diagnosis [4]. Pneumocystis jewel mostly occurs in preterm infants, malnourished infants, and immunosuppressed children and adults [5]. The first-line drug was compound sulfamethoxazole. After the return of BALF results in this patient, we added compound sulfamethoxazole tablets, and the subsequent review of chest CT suggested that the treatment was effective.
After the occurrence of lung infection, glucocorticoid gradually reduced, we stopped the third IFX, and considered thalidomide can be used for the treatment of refractory UC, so we gived thalidomide to control intestinal inflammation, and continue to use mesalazine. The stools was no significant abnormalities in the subsequent follow-up, and lung infection also be effectively controlled. In the future, when the patient’s pulmonary infection is stable, if the intestinal inflammation is repeated again, Verilizumab can be tried, but more experience will still need to be accumulated in the drug safety of the patient when combined with severe infection. We report this case to highlight clinicians should pay close attention to pulmonary opportunistic infection after the use of glucocorticoids, and biologic agents in UC treatment. In the process of moderate to severe UC treatment, if glucocorticoids, immunosuppressive agents and biological agents are uesd, we should be alert to opportunistic infection. We should combine the laboratory test results and the pathogen test results for a comprehensive judgment, timely choose reasonable and effective drug to control infection, and adjust the intestinal treatment, ultimately improve the prognosis of patients.
References
- Shan-Shan, Gong, Yi-Hong, et al. Nested case-control study on risk factors for opportunistic infections in patients with inflammatory bowel disease [J]. World journal of gastroenterology, 2019; 25: 2240-2250.
- Cohen RD, Bhayat F, Blake A, et al.The safety profile of vedolizumab in ulcerative colitis and Crohn’s disease.4 years of global post-marketing data [J]. J Crohns Colitis, 2020; 14: 192-204.
- Van der Have M, Belderbos TD, Fidder HH, et al. Screening prior to biological therapy in Crohn’s disease: adherence to guidelines and prevalence of infections. Results from a multicentre retrospective study [J]. Dig Liver Dis, 2014; 46: 881-886.
- Montagna MT, Lovero G, Coretti C, et al. SIMIFF study: Italian fungal registry of mold infections in hematological and non-hematological patients [J]. Infection, 2014; 42: 141-151.
- Yassin AF, Rainey FA, Steiner U. Nocardia cyriacigeorgici sp. nov [J]. Int J Syst Evol Microbiol, 2001; 51: 1419-1423.
- Barnaud G, Deschamps C, Manceron V, et al. Brain abscess caused by Nocardia cyriacigeorgica in a patient with human immunodeficiency virus infection [J]. Journal of Clinical Microbiology. Sept. 2005; 4895-4897.
- Cilloniz C, Dominedo C, Alvarez Martunez M J, et al. Pneumocystis pneumonia in the tweenty-dcentury, HIV-infected versus HIV-unifected patients [J]. Expert Rev Anti Infect Ther, 2019; 17: 787-801.