Japanese Journal of Gastroenterology Research
Short Report - Open Access, Volume 2
Rare case of right lower abdomen pain
Jinpeng Li; Gaofei Shen; Zhenzhen Liu; Fei Zhu; Huifen Lian; Junyi Zheng; Rui Huang*
Department of Gastroenterology, Xi’an People’s Hospital (Xi’an Fourth Hospital), Xi’an, Shaanxi, China.
*Corresponding Author : Rui Huang
Department of Gastroenterology, Xi’an People’s Hospital
(Xi’an Fourth Hospital), Xi’an, Shaanxi, China.
Email: sangyahr@163.com
Received : Mar 23, 2022
Accepted : Apr 14, 2022
Published : Apr 20, 2022
Archived : www.jjgastro.com
Copyright : © Huang R (2022).
Citation: Li J, Shen G, Liu Z, Zhu F, Huang R, et al. Rare case of right lower abdomen pain. Japanese J Gastroenterol Res. 2022; 2(6): 1075.
Clinical presentation
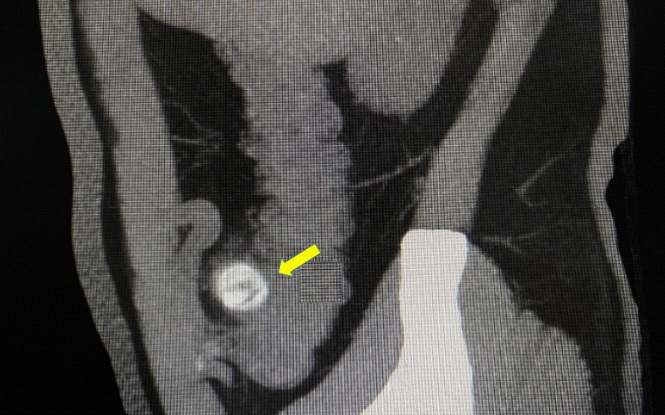
A 48-year-old male presented with mild right lower abdomen pain of 2 days duration, which was continue, without radiation. No accompanying symptoms such as fever, nausea, vomiting and diarrhea. His past medical history were hypertension and cholecystectomy. In addition, he has a history of constipation before cholecystectomy. He has no previous episodes of similar abdominal pain. Physical examination revealed abdominal tenderness in right lower quadrant. His blood routine and C-reaction protein examination were normal. During computed tomography scan of his abdomen (Figure 1,2) followed by colonoscopy, an unexpected finding was noted in caecum.
Question
What do the images show? What is the diagnosis?
Answer
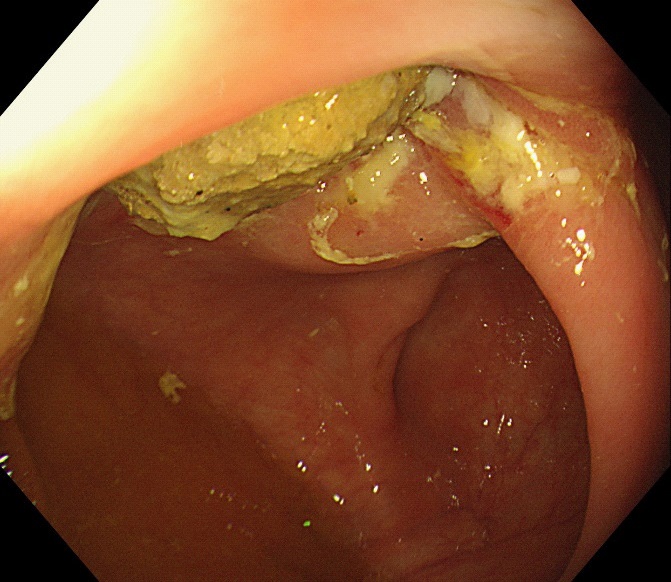
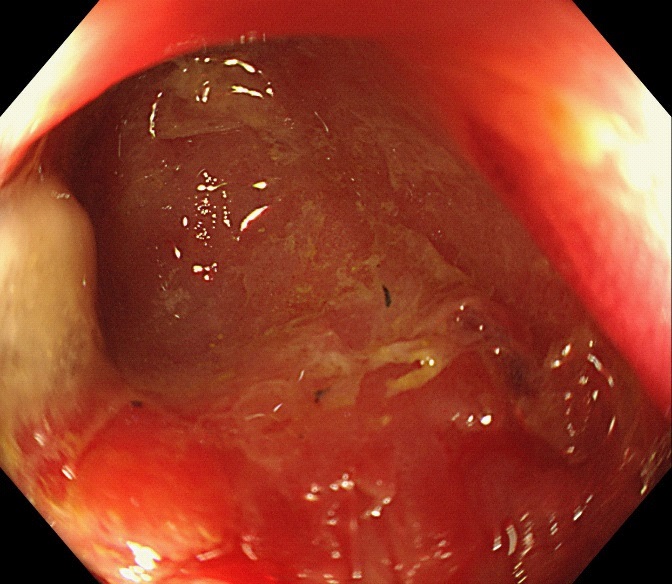
The computed tomography scan of abdomen showed about 20 mm X 20 mm circular high density shadow in right colon, which can be observed in colonic lumen but protruding out of the lumen. Colonoscopy (Figure 3) was also performed and the fecal impaction was identified in the cecal diverticulum above the ileocecal valve. The mucosa surrounding the diverticulum was hyperemic and edema. Than the fecalith was removed successfully with a foreign forceps under colonoscopy. The internal mucosa of the diverticulum was hyperemia, and no perforation was observed (Figure 4). The patient’s abdominal pain were relieved after endoscopic treatment. To prevent recurrence of the disease, surgical removal of the diverticulum was recommended but the patient was hesitant. There was no recurrence of abdominal pain and fecal impaction during 10 months follow-up.
Discussion
The disease mentioned above is called "Diverticular Disease". Diverticular which occurs when intestinal mucosa and submucosa herniate through defects in the muscle layer of the intestinal wall [1,2]. It remains asymptomatic in most individuals but 10%-25% of individuals will develop symptomatic diverticulosis, termed diverticular disease [3,4]. Diverticulitis is the most common complication of diverticulosis, and its pathophysiology is the obstruction of the diverticulum sac by fecalith or other foreign body (ingested bone, etc.), causing low-grade inflammation, congestion and further obstruction. More severe diverticulitis leads to hemorrhage, abscess, fistula, obstruction and/or or perforated [5]. In Western countries, 90% of cases of diverticulosis are found in the sigmoid or left colon [6]. In East Asia (Japan and Korea) diverticulosis is more common in the ascending or right colon (75%-85%) [7,8]. There is currently no clear answer to the reason for this difference. However, it is determined that factors such as age, genetics, and dietary structure affect the occurrence and development of diverticulosis [9].
This patient had persistent abdominal pain due to fecal incarcerate colonic diverticulum. Fecal impaction is defined as a large mass of compacted feces in the colon and has the potential to induce a serious medical condition such as bowel obstruction or abdomen pain. This is a typical colonic diverticulitis caused by fecalith: Colonoscopy found that the mucosa around the diverticulum was obviously hyperemia and edema, but the peripheral blood inflammatory indicators have not been shown. Fortunately, the timely treatment and treatment of the patient avoided the risk of colonic obstruction and even perforation. As shown in the diagnosis and treatment of this patient, imaging examinations (CT and MRI) have obvious advantages in early identification of diverticulitis caused by foreign body impaction [10]. For the treatment of such diverticulitis, colonoscopy is the first choice, showing great advantages [11]. But some complicated cases still require surgical operations [12]. In addition, it is still necessary to improve diet and lifestyle, strengthen exercise, and maintain smooth bowel movements [13].
To remove the incarcerated fecalith in colonic diverticulum by colonoscopy foreign forceps, there are the following considerations: a. Colonoscopy must fully observe the mucosal folds, especially the intestinal curvature; b. After finding a colonic diverticulum, pay attention to observe the diverticulum sac, and it is possible to find inflammation, foreign bodies; c. Colonoscopy to remove foreign bodies in colonic diverticulum requires better visual field exposure, careful manipulation, and may even require the help of digestive surgery.
References
- Rezapour M, Ali S, Stollman N. Diverticular Disease: An Update on Pathogenesis and Management J. Gut Gut Liver. 2018; 12: 125-132.
- Schieffer KM, Kline BP, Yochum GS, et al. Pathophysiology of diverticular diseaseJ.. Expert Rev Gastroenterol Hepatol. 2018; 12: 683-692.
- Tursi A, Scarpignato C, Strate LL, et al. Colonic diverticular diseaseJ.. Nat Rev Dis Primers. 2020; 6: 20.
- Parks TG. Natural history of diverticular disease of the colonJ. Clin Gastroenterol. 1975; 4: 53-69.
- Stollman N, Raskin JB. Diverticular disease of the colonJ. Lancet. 2004; 363: 631-639.
- Tursi A. Current and Evolving Concepts on the Pathogenesis of Diverticular DiseaseJ. J Gastrointestin Liver Dis. 2019; 28: 225- 235.
- Yamamichi N, Shimamoto T, Takahashi Y, et al. Trend and risk factors of diverticulosis in Japan: age, gender, and lifestyle/metabolic-related factors may cooperatively affect on the colorectal diverticula formationJ. PLoS One. 2015; 10: e0123688.
- Song JH, Kim YS, Lee JH, et al. Clinical characteristics of colonic diverticulosis in Korea: a prospective studyJ.. Korean J Intern Med. 2010; 25: 140-146.
- Kupcinskas J, Strate LL, Bassotti G, et al. Pathogenesis of Diverticulosis and Diverticular DiseaseJ. J Gastrointestin Liver Dis. 2019; 28: 7-10.
- Tursi A. Advances in the management of colonic diverticulitisJ. Cmaj. 2012; 184: 1470-1476.
- Tursi A. The role of colonoscopy in managing diverticular disease of the colonJ.. J Gastrointestin Liver Dis, 2015, 24(1): 85-93.
- Lock J, Wiegering A, Germer CT. Indications for surgical treatment of diverticular disease J. Chirurg; 2021; 92: 694-701.
- Strate LL. Lifestyle factors and the course of diverticular diseaseJ. Dig Dis. 2012; 30: 35-45.