Japanese Journal of Gastroenterology Research
Research Article - Open Access, Volume 2
Role of fatty acid binding protein 1 in non-alcoholic fatty pancreatic disease versus non-alcoholic fatty liver disease: An Egyptian pilot study
Reda Albadawy1*; Mohamed Kamel2; Marwa Matboli3; Ghadeer Masoud1
1 Departments of Hepatology, Gastroenterology Banha University, Egypt.
2 Departments of Radiology, Menofyia University, Egypt.
3 Departments of Biochemistry, Ain Shams University, Egypt.
*Corresponding Author: Reda Albadawy
Departments of Hepatology, Gastroenterology
Banha University, Egypt.
Email: reda.albadawy@fmed.bu.edu.eg
Received: Jan 10, 2022
Accepted: Mar 01, 2022
Published: Mar 08, 2022
Archived: www.jjgastro.com
Copyright: © Albadawy R (2022).
Abstract
Background & aim: Non Alcoholic Fatty liver Disease is health problem world wide including Egypt. By 2030 NAFLD will be the first indication for liver transplantation plus its cardiac mortality side effects. Non-alcoholic fatty pancreatic disease (NAFPD) comprises a wide spectrum of diseases from deposition of fat in the pancreas (fatty pancreas, pancreatic steatosis), to pancreatic inflammation (non-alcoholic steatopancreatitis), possible pancreatic fibrosis and pancreatic cancer. NAFPD also considered the mirror image of NAFLD due to the same origin of both. FABP1 is a 14-kDa protein that participates in fatty acid metabolism in the cytoplasm. Furthermore, FABP1 facilitates the transportation, storage, and utilization of fatty acids and their acyl-CoA derivatives and may exert a protective effect against lipotoxicity at the level of hepatocyte and enterocyte by facilitating their oxidation or incorporation into TGs and binding otherwise cytotoxic-free fatty acids. So the aim of the study to assess the diagnostic role of FABP1 as noninvasive biomarker in patients with NAFPD versus NAFLD.
Methodology: This was a cross sectional study, conducted on 88 Subjects (22 of them healthy with no DM or obese and 66 divided into 3 groups, DM or not obese or not each group 22, age, sex matched. All Subjects evaluated thorough full history taking, clinical examination BMI, biochemical assessment for liver function tests and lipid profile. Abdominal ultrasound for grading of both NAFLD and NAFPD from (0-3). FABP1 was assessed using ELISA kits.
Result: There was statistical significant for all investigations between groups except, albumin, TG, Hb and plt. Grads of NAFPD was of highly statistical significant, p= 0.001 while grades of NAFLD was 0.01. There was progress of fatty pancreas grading more than fatty liver. FBP1 was of statistical significant in both NAFPD & NAFLD, p= 0.01.
Conclusion: FABP1 is a good biomarker, simple, noninvasive and unique for diagnosis of fatty pancreas especially as well as fatty liver
Keywords: non-alcoholic; fatty pancreas disease; Fatty acid-binding protein 1; trigylceride (TG).
Abbreviations: NAFPD: Non-Alcoholic Fatty Pancreas Disease; FABP1: Fatty Acid Binding Protein 1; BMI: Body Mass Index; ELISA: Enzyme-Linked Immunosorbent Assay.
Citation: Albadawy R, Kamel M, Matboli M, Masoud G. Role of fatty acid binding protein 1 in non-alcoholic fatty pancreatic disease versus non-alcoholic fatty liver disease: An Egyptian pilot study. Japanese J Gastroenterol Res. 2022; 2(4): 1065.
Introduction
Nonalcoholic fatty pancreas disease (NAFPD) is an excessive lipid accumulation in the pancreas in the absence of significant alcohol intake [1]. This condition was first described by Schaefer in 1926 [2], and later by Ogilvie In 1933 who used the term ‘pancreatic lipomatosis’ to represent the pathological process of excessive fat storage in the pancreas [3]. On the contrary, to the non-alcoholic fatty liver disease (NAFLD), the potential systemic and local consequences of excessive fat accumulation in the pancreas have not been well-established [4].
Prevalence of NAFPD has been reported in Asia as well as in Western countries. In Taiwan, Wang et al. reported that 16% of Chinese population had fatty pancreas [5]. In Indonesia, which represents the biggest Southeast Asian country, the prevalence of NAFPD in the medical check-up population was 35%. Up to the moment no Egyptian study done about NAFPD and its relation to Obesity or DM with its complications [6]. Pancreatic fat content may play a role in several local pathological processes such as pancreatic cancer or subtypes of pancreatitis [7]. NAFPD may allegedly develop into chronic pancreatitis and further leads to pancreatic cancer, and facilitates its dissemination to date, the pathophysiology of NAFPD remains unclear. There are two potential mechanisms for pancreatic fat accumulation: (i) death of acinar cells, followed by replacement with adipose tissue; and (ii) intracellular triglyceride accumulation associated with positive energy balance [8]. Fatty pancreas is an emergent problem that need new markers that can be used as a simple non-invasive biomarker to aid in diagnosis to be added to the investigation other than ultrasound.
Fatty acid-binding proteins (FABPs) are a family of small and highly conserved lipid chaperone molecules with highly varied functions [9]. FABPs hold promise as markers of tissue injury. When there is ongoing damage, FABP is measurable in serum. The designation of each of the proteins in this family has been taken from the tissue where it was originally isolated, and key members of this group of proteins include liver fatty acid-binding protein (L-FABP), intestinal FABP, heart FABP and epidermal FABP [10]. FABP1 facilitate the transportation, storage and utilization of fatty acids and their acyle-coA derivatives at the level of hepatocyte and intestine and may exert a protective effect against lipotoxicity by facilitating their oxidation or incorporation into TGs and binding other wise cytotoxic-free fatty acids [11]. We suggested that FABP may be adiagnostic marker for NAFPD. This study aimed to determine the role of FABP1 in patients with Non-Alcoholic Fatty Pancreatic Disease versus Non Alcoholic Fatty liver Disease.
Patients and methods
Study population
This was a cross sectional study, conducted on 88 Subjects who attended to AL Helal Hospital in Shebin EL Kom, Menoufia during the period from March 2020 till December 2020. This study was approved by the Ethical Committee of Benha Faculty of medicine, Informed written consents was taken from all participants in this study after explaining the aim for them. This study population was devided as follow:
Group A: included 22 subjects Normal BMI, Non-diabetics.
Group B: included 22 patients Normal BMI, Diabetics.
Group C: included 22 patients with BMI over 25, Non-diabetics.
Group D: included 22 patients with BMI over 25, Diabetics.
Inclusions criteria: Normal BMI and obese peoples with and without DM type 2. All subjects aged from 18-70 years old.Both sex were included.
Exclusions criteria: Patients with history of Chronic pancreatitis or previous attacks of pancreatitis and admission to the hospital. Patients with viral hepatits B, C, autoimmune and alcoholic. The patients were evaluated clinically thorough Full medical history, Full clinical examination: as Blood pressure, body mass index (BMI) = weight (Kgm)/ height (meter)2 >30 kg/ m2 , laboratory Investigations as follow Complete blood count (CBC) and ESR. Fasting blood sugar, HbA1c%, HCV antibody & HBVs antigen, Liver Profile including alanine amino transferase, aspartate amino transferase, gamma glutamyl transpeptidase, alkaline phosphatase (ALT, AST, GGT, ALP) serum bilirubin, and serum albumin. Lipid profile including (cholesterol, triglycerides, HDL, and LDL). Serum Insulin level for calculating insulin resistance (IR), HOMA-IR was assessed using the given mathematical equation; HOMA-IR=fasting insulin (mU/ml) x fasting plasma glucose (mmol/l)/22.5 [12].
Fatty Acid Binding protein1 (FABP1: FABP was evaluated by the enzyme-linked immunosorbent assay (ELISA) and the deviation from the normal will be correlated with other investigations and clinical manifestations of the subjects. Abdominal Ultrasound using Toshiba.
The pancreas and liver echogenicity was also classified into 4 grades from 0-3 [13]
- Grade 0, the pancreas echogenicity was similar to the kidney parenchymal.
- Grade1, pancreas echogenicity was slightly higher than in the kidney if the operator can see both in the same view in the transverse epigastric scan with slight move to the right, if the pancreas and kidney could not be displayed in the same screen, the radiologist compared the kidney with the liver and then compared the liver with the pancreas.
- Grade 2, a substantial increase in pancreas echogenicity but lower than the retroperitoneal fat echogenicity.
- Grade 3, the pancreas echogenicity was similar to or higher than the retroperitoneal fat.
NAFPD was diagnosed when the pancreas appeared as grade 1 to 3. -Grades of fatty liver as per literature.
Statistical analysis
Data were collected, tabulated, statistically analysed using Statistical Package of Social Science (SPSS) version 22 to obtain Descriptive data and Analytical data.
Descriptive statistics
In which quantitative data were presented in the form of mean ( ), standard deviation (SD), range, and qualitative data were presented in the form numbers and percentages.
Analytical statistics
Used to find out the possible association between studied factors and the targeted disease. The used tests of significance included:
• Chi-square test (χ2): was used to study association between two qualitative variables.
• ANOVA (f) test: is a test of significance used for comparison between three or more groups having quantitative variables.
• Kruskal-Wallis test (nonparametric test): is a test of significance used for comparison between three or more groups not normally distributed having quantitative variables.
• Spearman’s correlation (r): is a test used to measure the association between two quantitative variables not normally distributed.
A P value of >0.05 was considered statistically non-significant while P value of <0.05 was considered statistically significant and P value of <0.001 was considered statistically highly significant.
Results
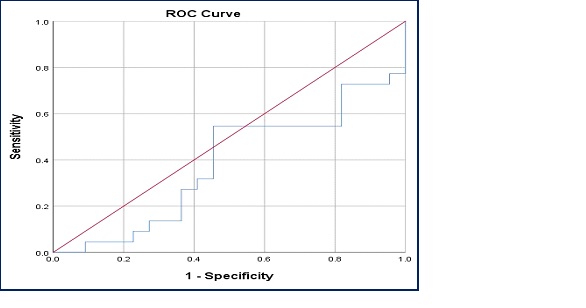
The studied groups were 88 patients. The mean age of the studied patients was 44.08 ± 12.41 years; mean of BMI was 29.73 ± 8.15 kg/m2. 72% of patients were males and 27% were females. 21.6% of them were smokers, 17.1% had hypertension. 71.6% were Manual worker and 27.4% were employer. Also, most of the studied patients (84.1) were living in urban areas. There was statistically significant difference between studied groups as regard almost all studied parameters and p value ranged from 0.05 to 0.001 for most of laboratory parameters, while there is no statistically significant difference between studied groups regarding Hb%, TG, PLT count and S. albumin (Table 1). The level of FABP1 increased in non diabetic patients with BMI >25 with statistically significant difference to other groups and was of statistical significant p =0.01 between all groups (Table 2). There was increased grading of fatty pancreas compared to fatty liver from grade 1 to grade 3 (Table 2), this mean that NAFPD could be started before NAFLD or it can even started before NAFLD. Another explanation is the association between NAFPD and NAFLD as a metabolic lipid disorder of one disease. At cut off 0.758 the sensitivity of FABP1 in prediction of fatty pancreas as well as fatty liver was (68.2%), specificity (45.5%) and area under the curve was 0.618 in diabetics, non diabetics with normal BMI (Figure 1). At cut off 0.80 the sensitivity of FABP1 in prediction of fatty pancreas and fatty liver was (54.5%), specificity (54.5%) and area under the curve was 0.382 in non diabetics, diabetics with BMI >25, (Figure 2).
Table 1: The demography and laboratory investigations of the study groups.
|
Group A (22) Normal subjects |
Group B (22) |
Group C (22) |
Group D (22) |
Statistical test (F) |
P value |
||||
Mean |
±SD |
Mean |
±SD |
Mean |
±SD |
Mean |
±SD |
|||
Age |
41.55 |
13.78 |
42.82 |
11.23 |
44.27 |
13.06 |
47.68 |
11.39 |
1.0 |
0.40 |
Gender |
|
|
|
|
|
|
||||
BMI |
20.73 |
2.31 |
36.45 |
5.63 |
24.59 |
0.67 |
37.14 |
4.49 |
105.68 |
<0.001** |
SBP |
115.91 |
12.21 |
126.82 |
19.12 |
122.73 |
18.56 |
128.14 |
15.59 |
2.41 |
0.07 |
DBP |
76.27 |
13.97 |
81.36 |
11.25 |
81.32 |
13.17 |
82.59 |
9.75 |
1.17 |
0.33 |
WBCs |
6.2 |
2.21 |
6.29 |
2.14 |
6.85 |
2.35 |
8.51 |
2.52 |
4.71 |
0.004** |
Hb |
12.48 |
1.56 |
12.48 |
1.78 |
12.89 |
1.64 |
12.63 |
1.75 |
0.29 |
0.83 |
PLT |
251.77 |
63.09 |
231.0 |
57.83 |
213.95 |
83.61 |
240.64 |
73.11 |
1.15 |
0.33 |
FBG |
95.18 |
7.66 |
97.95 |
6.37 |
195.55 |
74.0 |
207.32 |
78.05 |
27.83 |
<0.001** |
HbA1c |
4.24 |
0.18 |
4.26 |
0.26 |
8.15 |
1.75 |
8.65 |
1.90 |
74.99 |
<0.001** |
ALT |
24.27 |
10.63 |
56.18 |
13.25 |
39.5 |
23.18 |
41.41 |
19.94 |
12.25 |
<0.001** |
AST |
20.86 |
9.67 |
55.27 |
14.56 |
37.77 |
33.29 |
59.82 |
25.41 |
13.53 |
<0.001** |
GGT |
29.68 |
11.75 |
76.45 |
13.36 |
59.41 |
23.32 |
72.64 |
15.02 |
36.45 |
<0.001** |
ALP |
85.55 |
20.57 |
161.64 |
17.81 |
132.0 |
42.61 |
147.64 |
19.66 |
32.7 |
<0.001** |
T bilirubin |
0.79 |
0.21 |
0.79 |
0.20 |
0.87 |
0.25 |
0.98 |
0.19 |
4.08 |
0.009** |
D bilirubin |
0.42 |
0.12 |
0.26 |
0.19 |
0.41 |
0.16 |
0.44 |
0.14 |
6.13 |
0.001** |
Albumin |
4.29 |
0.28 |
4.11 |
0.29 |
3.86 |
0.38 |
5.75 |
8.33 |
0.91 |
0.44 |
Cholesterol |
293.86 |
125.33 |
357.41 |
158.83 |
201.5 |
65.18 |
234.36 |
99.92 |
7.53 |
<0.001** |
TG |
100.27 |
26.66 |
101.91 |
30.34 |
102.32 |
34.49 |
133.32 |
113.0 |
1.43 |
0.24 |
HDL |
32.45 |
8.78 |
32.23 |
6.87 |
37.09 |
7.46 |
37.5 |
9.26 |
2.72 |
0.049* |
Table 2: The grades of Fatty pancreas and fatty liver and the level of FABP1 in all groups.
|
Group A (22) Normal subjects |
Group B (22) | Group C (22) | Group D (22) | Statistical test (F) | P value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
Mean |
±SD |
Mean |
±SD |
Mean |
±SD |
Mean |
±SD |
|||
FABP1 |
0.99 |
0.71 |
1.42 |
1.12 |
0.60 |
0.24 |
0.85 |
0.85 |
4.06 |
0.01* |
Grades on pancreas |
|
|
|
|
|
|
||||
Grades on Liver |
|
|
|
|
|
|
||||
Discussion
In this study the mean age of the studied patients was (44.08 ± 12.41) years (Table 1), this is the golden age of the start of metabolic diseases in general. This is in agree with El-Badawy, et al who found the mean age of patients with NAFPD was (44.15 ± 10.24) years which was significantly higher compared to non NAFPD subjects (39.12 ± 11.17) [14]. This also came in agreement with a result of study by Wang, who showed a positive correlation between age and fatty pancreas, with increasing prevalence of fatty pancreas with age [15]. Also, it has been reported by Lesmana et al, [6] that presence of fatty pancreas was significantly associated with age >35 years. Therefore, older age is considered as an important risk factor of NAFPD. In the current study, NAFPD was more frequently in males than females (64 versus 24) with male to female ratio (2.6:1). This might be related to lipid metabolism dysfunction being aggravated by age-related slowing of metabolism and aggravation of ectopic fat deposition caused by prolonged dyslipidaemia [16]. NAFPD can started before NAFLD or both of them can started together with one preceded other, as per literature NAFPD more serious too that NAFLD. So the need for early diagnosis by biomarker as pancreas not easily seen by ultrasound is highly needed. The male predominance came in agreement with Lesmana, who reported an association of male gender and NAFPD [6]. It was hypothesized that men are at higher risk to develop NAFPD because they had more visceral (abdominal) fat deposition while women had more subcutaneous (gluteal femoral) lipid deposition.In the present study, the mean of BMI was (29.73 ± 8.15) (Table 1). This agreed with El-Badawy who showed that, the presence of the disease was associated with higher values of BMI with statistically significant differenc. Between fatty pancreas group and non-fatty pancreas group, the mean BMI was (30.4 kg/m2 vs. 27.3 kg/m2, P < 0.001) [14].
Also the current study showed there was statistically significant difference between studied groups as regard ALT, AST, GGT, ALP, T. bilirubin, D. bilirubin which were higher in diabetic patient either with normal BMI or with BMI >25 kg/m2 in (Table 1). This in line with Lee, who reported a correlation between fatty pancreas and liver enzymes including AST, ALT, and γ GGT as compared to the normal pancreas group [4]. On the other hand, Wang, showed that no significant associations were found between fatty pancreas and AST, ALT, and γ GGT levels [5]. The present study revealed that high levels of S. cholesterol in diabetics and non-diabetics with normal BMI was statistically significant difference (Table 1). This came in line with Wang who reported that fatty pancreas group was characterized by a significantly higher total cholesterol (P=0.001), TG (P<0.001), LDL-C (P<0.001), and VLDL-C values (P< 0.001) and by a significantly higher Cholesterol/HDL (P=0.007) and LDL/ HDL ratios (P=0.024) [5].
Table (2) show statistical significant difference for fatty pancreas in all groups especially in normal subjects, 6 patients with no fatty pancreas while 8 patients with no fatty liver, this mean that fatty pancreas started before fatty liver. FABP1 of statistical significant with groups.
The level of FABP1increased in non diabetic patients with BMI >25 with statistically significant difference to other groups (Table 2). This came in line with Abdelkader who reported that there was statistically significant difference positive correlation between FABP1 and BMI and fasting blood sugar [17]. FABP1 is statistically significant in both NAFPD and NAFLD (Table 3).
Table 3: Relation between FABP1 level and different grades of fatty pancreas among the studied groups.
| FABP1 | ANOVA test | |||||||
| Mean ±SD | Range | F | P value | |||||
| Non-Diabetics (n=44) | Normal BMI | Grades on pancreas | 1.48 | 0.25 | ||||
| No | 1.07 | 0.87 | 0.36 | 2.79 | ||||
| I | 0.67 | 0.17 | 0.46 | 0.89 | ||||
| II | 0.75 | 0.40 | 0.11 | 1.36 | III | 1.49 | 0.98 | 0.70 | 2.58 |
| BMI>25 | Grades on pancreas | 7.03 | 0.005** | |||||
| I | 0.51 | 0.13 | 0.36 | 0.70 | ||||
| II | 0.43 | 0.15 | 0.16 | 0.59 | III | 0.76 | 0.23 | 0.35 | 1.24 |
| Diabetics (n=44) | Normal BMI | Grades on pancreas | St t= 0.06 | 0.95 | ||||
| II | 1.39 | 0.97 | 0.70 | 3.0 | ||||
| III | 1.43 | 1.21 | 0.41 | 4.31 | ||||
| BMI>25 | Grades on pancreas | St t= 0.59 | 0.56 | |||||
| II | 0.62 | 0.20 | 0.38 | 0.82 | ||||
| III | 0.90 | 0.93 | 0.29 | 4.41 | ||||
Table (3) show statistical significant in group non DM withBMI > 25 kg/m2. This group also have patients with NAFLD which mean the high value of use FABP1 as biomarker in both NAFPD and NAFLD.
Conclusions
There was association between Non- alcoholic fatty pancreas and diabetes mellitus with increasing grading of fatty pancreas. Significant increase of FABP in different grades of fatty pancreas. We suggest that FABP may be a good marker for diagnosis of NAFPD.
Declarations
Acknowledgment: To Academic Scientific Research & Technology (ASRT)/Jesor project No /5269 for funding.
Funding: This research was funded from Academic Scientific Research & Technology Jesor project No/5269/2019.
References
- Alempijevic T, Dragasevic S, Zec S, Popovic D, Milosavljevic T. Nonalcoholic fatty pancreas disease. Postgrad Med J. 2017; 93: 226-230.
- Schaefer JH. The normal weight of the pancreas in the adult human being: A biometric study. Anat Rec. 1926; 32: 119-32.
- Ogilvie RF. The islands of langerhans in 19 cases of obesity. J Pathol Bacteriol. 1933; 37: 473-481.
- Lee JS, Kim SH, Jun DW, Han JH, Jang EC, Park et al. Clinical implications of fatty pancreas: correlations between fatty pancreas and metabolic syndrome. World journal of gastroenterology: WJG. 2009; 15: 1869.
- Wang CY, Ou HY, Chen MF, Chang TC, Chang CJ. Enigmatic ectopic fat: prevalence of nonalcoholic fatty pancreas disease and its associated factors in a Chinese population. J Am Heart Assoc. 2014; 3: 297-304.
- Lesmana CR, Pakasi LS, Inggriani S, Aidawati ML and Lesmana LA. Prevalence of Non-Alcoholic Fatty Pancreas Disease (NAFPD) and its risk factors among adult medical checkup patients in a private hospital: a large cross-sectional study. BMC gastroenterology. 2015; 15: 174.
- Mathur A, Zyromski N, Pitt H, Walker J, Saxena R, Lillemoe K et al. Pancreatic Steatosis Promotes Dissemination and Lethality of Pancreatic Cancer. Southern Surgical Association article. 2009; 208: 989-994.
- Smits MM, van Geenen EJ. The clinical significance of pancreatic steatosis. Nat Rev Gastroenterol Hepatol. 2011; 8: 169-177.
- Amiri M, Yousefnia S, Forootan FS, Peymani M, Ghaedi K, Esfahani MH. Diverse roles of fatty acid binding proteins (FABPs) in development and pathogenesis of cancers. Gene. 2018; 676: 171-83.
- Abdulaziz BA, Abdu SA, Amin AM, El Menyawi AK, Ahmed A, Khalil MA et al. Assessment of Liver Fatty Acid Binding Protein (L-FABP) as a Diagnostic Marker in NonAlcoholic Fatty Liver Disease. Open Journal of Gastroenterology. 2019; 9: 113-24.
- Wang G, Bonkovsky HL, de Lemos A, Burczynski FJ. (2015): Recent insights into the biological functions of liver fatty acid binding protein 1. Journal of lipid research. 2015; 56: 2238-47.
- Gutch M, Kumar S, Razi SM, Gupta KK, Gupta A. (2015): Assessment of insulin sensitivity/resistance. Indian journal of endocrinology and metabolism. 2015; 19(1): 160.
- Marks WM, Filly RA, Callen PW. Ultrasonic evaluation of normal pancreatic echogenicity and its relationship to fat deposition.Radiology. 1980; 137: 475-9.
- El-Badawy R, Yousef A, Elkholy H and Mustafa A. Studying the Association between Non-Alcoholic Fatty Pancreatic Disease and Non-Alcoholic Fatty Liver Disease. Benha Medical Journal. 2020.
- Wang D, Yu XP, Xiao WM, Jiao XP, Wu J, Teng DL et al. Prevalence and clinical characteristics of fatty pancreas in Yangzhou, China: A cross-sectional study. Pancreatotomy. 2018; 18: 263-8.
- Wallace TM, Levy JC, Matthews DR. An increase in insulin sensitivity and basal betacell function in diabetic subjects treated with pioglitazone in a placebo-controlled randomized study. Diabet Med. 2004; 21: 568-76.
- Abdelkader A, Al-Dahshan M, Ali M, Othman M, Al-Zohairy Y. Non Alcoholic Fatty Pancreatic Disease Significance, Importance and Risk factors. International Journal of Science and Research (IJSR). 2019; 7: 583.