Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 2
Endoscopic management of ulcerated giant intramural lipoma causing colo-colic intussusception
Syed Afzal ul Haq Haqqi1*; Syed Zea ul Islam Farrukh2; Arif Rasheed Siddiqui3; Saad Khalid Niaz4; Ali Kamran5
1 Fellowship, Therapeutic Endoscopy (Hongkong), Consultant Gastroenterologist & Hepatologist Patel, Hospital Karachi, Pakistan.
2 Fellowship, Endoscopy United Kingdom, Consultant Gastroenterologist & Hepatologist, Patel Hospital Karachi, Pakistan.
3 Consultant, Gastroenterologist & Hepatologist, Patel Hospital Karachi, Pakistan.
4 Consultant, Gastroenterologist & Hepatologist, Patel Hospital Karachi, Pakistan.
5 Consultant, General Surgeon, Patel Hospital Karachi, Pakistan.
*Corresponding Author: Syed Afzal ul Haq Haqqi
Consultant, Gastroenterologist & Hepatologist, Patel
Hospital Karachi, Pakistan.
Email: afzalhaqqi@hotmail.com
Received: Dec 28, 2021
Accepted: Feb 21, 2022
Published: Feb 28, 2022
Archived: www.jjgastro.com
Copyright: © Haqqi SA (2022).
Abstract
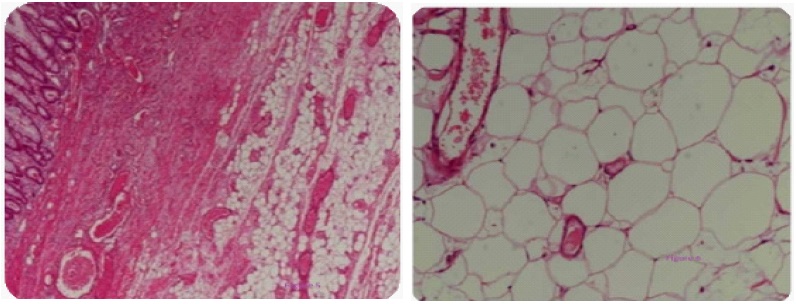
Colonic lipomas are extremely rare non epithelial tumors, usually small and located in the right colon. They may also act as unusual pathological lead point for intussusceptions, especially in the descending colon. We describe the case of a 70 years old lady with no known comorbids. She presented with severe abdominal pain that stated suddenly three hours prior to her presentation in the Emergency Room, CT Abdomen showed Colo-colic intussusception secondary to possible lipoma as a lead point, initially planned for surgical intervention but patient got better and planned Colonoscopy which showed partially obstructing large pedunculated Kudos 1p polyp in descending colon (Figures 1 and 2), endoscopic hot snare en bloc polypectomy was performed successfully entire polyp of 7 X 3.5 X 3 (Figure 4) cm was retrieved. The post endoscopic period went uneventful and histology confirms the diagnosis of lipoma (Figures 5 and 6).
Manuscript classifications: colonoscopy; endoscopy; intussusception; polypectomy.
Keywords: intussusception; lipoma; computed tomography; endoscopic management.
Citation: Haqqi SA, Farrukh S, Siddiqui AR, Niaz SK, Kamran A. Endoscopic management of ulcerated giant intramural lipoma causing colo-colic Intussusception. Japanese J Gastroenterol Res. 2022; 2(3): 1063.
Introduction
Intussusception (L. “intus”- within and “suscipere”- to receive) has been acknowledged clinical entity since the late 16th century when it was described by Barbette of Amsterdam and subsequently described in more brilliant fashion by John Hunter in 1789 [1]. Colonic lipomas are one of the extremely rare non epithelial tumors, with a documented incidence ranging from 0.15% to 4.4% [2,3]. Majority of colonic lipomas are asymptomatic and small (less than 2 cm), Colonic lipomas that are larger than 4 cm are termed “Giant Polyp” [2]. Seventy five percent of Giant polyps are symptomatic [2,4,5], usually seen in the right colon, but can be uncommon pathological lead points for intussusception especially in descending colon. Although Intussusception is a common cause of abdominal pain in children, it is not that commonly seen in adult population. Intussusception results in 1% of all bowel obstruction in adults. Colo-colic intussusception in contributes to 17% of all intestinal intussusceptions in adults [6,7]. Clinically, they can mimic clinical manifestations of colonic carcinoma, such as bleeding, obstruction and abdominal pain [6,7]. In this report, we describe a 70-year-old female who developed a colo-colonic intussusception secondary to a Giant polyp located in the descending colon. We also present a review of the literature.
Case presentation
67 years old female no known co-morbids presented to emergency room with episodic severe abdominal pain and vomiting for the last 2 weeks, she brought a CT Abdomen with her which was done a week back, which showed colo-colic intussusception in left colon secondary to possible lipoma as a lead point, initially planned for surgical intervention but patient got better and obstruction was relieved by initial conservative management, she was sheduled for colonoscopy, which showed partially obstructing large pedunculated Kudos 1p polyp in descending colon (Figures 1 and 2). Pros and cons of endoscopic polypectomy were discussed with patient and patient’s family with possible complications of this giant polyp removal was explained in detail, patient and the patient’s family opted for the endoscopic management and informed consent was taken for the same. Elective hot snare en bloc polypectomy was performed uneventfully entire polyp of 7 X 3.5 X 3 cm (Figure 4) was retrieved successfully. The post endoscopic period went uneventful and histology confirms the diagnosis of lipoma. Patient visited our outpatient clinic at 2 weeks and 4 weeks post procedure, she remained well throughout with no abdominal pain and no drop in haemoglobin.
Discussion
Intestinal Intussusception occurs rarely in adult population, resulting in 1% of bowel obstructions and 0.003% to 0.02% of all hospital admissions [8]. In most cases of adult colonic intussusceptions (65-70%), the underlying cause is a primary carcinoma [9]. Colonic Lipomas could be a very rare entity causing colonic intsusseseption, found mostly in women with a peak incidence between 50 and 60 years old [10]. Occasionally patients presented mostly with intermittent abdominal pain, constipation and obstruction as we encountered similar symptoms in our patient as well. Colonic lipomas can also be pedunculated, and endoscopy reveals ulceration or necrosis of the mucosa overlying this polypoid lesion [11], as in our case. Surgery is generally recommended for colonic lipomas that are greater than 2 cm [11] in size. Endoscopic removal is recommended for polyps smaller than 2 cm in size [6]. The endoscopic removal of colonic lipoma of even up to 3.8 cm has been performed [12]. The risks of endoscopic removal of larger lesions (>2 cm in diameter) include perforation because the adipose tissue is an inefficient conductor for electric current and prolonged cutting time [13]. However, there are multiple reports demonstrating successful endoscopic removal with acceptable complication rates for large colonic lipomas. Incomplete removal by endoscopic techniques warrants a surgical removal of this pathology [14]. Our patient opted for endoscopic removal of large pedunculated polyp as she symptomatically improved; she has also given the consent of laporatomy in case of complication like bleeding or perforation.
Conclusion
Colonic Lipomas are rare clinical entity and mostly asymptomatic but giant lipomas can be symptomatic and can lead to colo-colonic intussusception in adults. Endoscopic removal of giant polyp in our elderly patient avoided the left hemicolectomy. Safe polypectomy in experienced hands is an excellent alternative to surgery, avoiding long stay of hospitalization and post surgical morbidity and could be taken as first line approach for the treatment of giant polyps provided surgical support next door.
Declarations
Consent: Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Ethical Approval: Not apply.
Funding: No Funding.
Author contributions
1) Syed Afzal Haqqi- Performed colonoscopy and polypectomy, Principle Idea, data collection and revision of final work
2) Syed Zea-ul Islam Farrukh- Assist Colonoscopy, conception of work, Data collection
3) Arif Rasheed Siddiqui- Manuscript writing and literature search
4) Saad Khalid Niaz- Supervise the Procedure and critical revision of final work
5) Ali Kamran- On call Surgeon
Conflict of interest: None.
References
- Hunter J. On introsusception. Trans SocImprov Med Surg Knowledge 1793; 1: 103.
- Paskauskas S, Latkauskas T, Valeikaite G, Parseliunas A, Svag zdys S, Salad zinskas Z, et al. Colonic intussusception caused by colonic lipoma: a case report. Medicina. 2010; 46: 477e81.
- Megaly M, Yacoub G. Transverse colon submucosal lipoma presenting withcolocolic intussusception. ACG Case Rep J. 2016; 3: 158e9.
- Chiba T, Suzuki S, Sato M, Tsukahara M, Saito S, Inomata M, et al. A case of alipoma in the colon complicated by intussusception. Eur J GastroenterolHepatol. 2002; 14: 701e2.
- Bahadursingh AM, Robbins PL, Longo WE. Giant submucosal sigmoid colon lipoma. Am J Surg. 2003; 186: 81-2.
- Mouaqit O, Hasnai H, Chbani L, Oussaden A, Maazaz K, Amarti A. Pedunculatedlipoma causing colo-colonic intussusception: a rare case report. BMC Surg. 2013; 13: 51.
- De Figueiredo LO, Garcia DPC, Alberti LR, Paiva RA, Petroianu A, Paolucci LB, et al. Colocolonic intussusception due to large submucous lipoma: a case report open access [Internet] Int J Surg Case Rep. 2016; 28: 107e10
- Ouadii Mouaqit, Hafid Hasnai, Leila Chbani, Abdelmalek, Khalid Maazaz, et al. Pedunculated lipoma causing colo-colonic intussusception: a rare case report. BMC Surgery. 2013, 13: 51
- Wang N, Cui XY, Liu Y, Long J, Xu HY, Guo RX, Guo KJ. Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol. 2009, 15: 3303-3308.
- Ghidirim G, Mishin I, Gutsu E, Gagauz I, Danch A, Russu S. Giant submucosal lipoma of the cecum: report of a case and review of literature. Rom J Gastroenterol. 2005; 14: 393-396.
- Atmatzidis S, Chatzimavroudis G, Patsas A, Papaziogas B, Kapoulas S, Kalaitzis S, et al. Pedunculated cecal lipoma causingcolocolonic intussusception. A rare case report.Case Rep Surgry. 2012; 3: 279213.
- Kim CY, Bandres D, Tio TL, Benjamin SB, Al-Kawas FH. Endoscopic removal of large colonic lipomas.Gastrointest Endosc. 2002; 55: 929-31.
- Katsinelos P, Chatzimavroudis G, Zavos C, et al. Cecal lipoma with pseudomalignant features: a case report and review of the literature. World J Gastroenterol. 2007; 13: 2510-3.
- Jiang L, Jiang L, Li F, Ye H, Li N, Cheng N, et al. Giant submucosal lipoma located in the descending colon : a case report and review of the literature. World J Gastroenterol. 2007; 13: 5664.