Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 2
Biliary aspergillosis: Unusual presentation with elevated CA19.9
Blagica Krsteska*; Boro Ilievski; Slavica Kostadinova- Kunovska; Rubens Jovanovic
Institute of Pathology, Faculty of Medicine, Ss. Cyril and Methodius University in Skopje, North Macedonia
*Corresponding Author : Blagica Krsteska
Institute of Pathology, Faculty of Medicine, Ss. Cyril and Methodius University in Skopje, North Macedonia
Email: blagicadr@yahoo.com
Received : Dec 14, 2021
Accepted : Jan 07, 2022
Published : Feb 03, 2022
Archived : www.jjgastro.com
Copyright : © Krsteska B (2022).
Abstract
Aspergillosis is a disease caused by a common mould Aspergillus with a wide variety of clinical syndromes. Invasive aspergillosis is the most severe form and usually occurs in immunocompromised patients. Hepatobiliary aspergillosis is uncommin condition encountered in immunocompetent patients. We report a case of aspergillosis in Ampulla of Vater with suspected malignancy due to elevated tumor marker CA19.9, jaundice and high values of liver enzymes. Diagnosis was confirmed by pathohistology and histochemical stain Grocott methenamine silver (GMS).
Keywords: aspergillosis; aspergillus; cholangitis; pancreatic carcinoma; ampulla of vater.
Citation: Krsteska B, Ilievski B, Kunovska SK, Jovanovic R. Biliary aspergillosis: Unusual presentation with elevated CA19.9. Japanese J Gastroenterol Res. 2022; 2(2): 1057.
Introduction
Aspergillus can cause a range of clinical manifestations which differ between patients according the localization and extent of the disease. The best known and most frequent presentation is pulmonary aspergillosis in noninvasive, invasive, chronic or allergic form. There is localized group that incorporates aspergillosis of paranasal sinuses and skin. The last important manifestation is disseminated aspergillosis, caused by hematogenous spread to different visceral organs [1]. Aspergillus fumigatus is responsible for 90% of invasive human aspergillosis with still high mortality rate [2]. Hepatobiliary aspergillosis is uncommon condition that can be found in several forms, many of which in immunocompetent patients, in patients after liver transplantation, or in patients with cholangitis and stone disease [3,4]. Here, we present a case of aspergillosis of Ampulla of Vater in a middle-aged patient with no previous clinically manifest fungal disease or liver damage.
Case presentation
A 49-year-old man was admitted to University Clinic for gastroenterology in March 2021 due to pain in the right hypochondriac region and jaundice. Laboratory results showed high CRP 62 mg/L, high cholestatic parameters ALP 292 UI/L and GGT 592 U/L, elevated AST 83 U/L, ALT 155 U/L, increased CA19.9 > 1000 U/ml (Table 1). An ultrasound and a PCR test for COVID 19 were indicated. Family history was negative and no relevant information for the current condition was obtained.
Diagnostic procedures
Ultrasound showed dilatation of intrahepatic biliary ducts, distal common bile duct with diameter of 15 mm visualized up to prepancreatic portion. Head of pancreas was hard to define and not visualized. The gallbladder was enlarged. Liver and spleen presented regular morphology. No ascites in peritoneal cavity was found. A papillotomy was performed and a billiary stent was placed. A malignant neoplasm of head of pancreas was suspected. The PCR test for COVID 19 was negative.
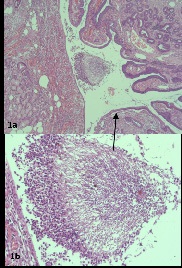
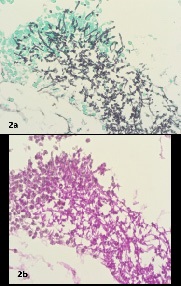
In April 2021 the patient was admitted to University Clinic for abdominal surgery for surgical treatment and Whipple procedure was performed with lymphadenectomy from portal vein and right hepatic artery. The specimen was send to Institute of pathology for diagnosis. On gross dissection, the head of pancreas measured 6X6,5X3,5 cm, the pancreatic part of common bile duct and ampulla of Vater had thick wall and narrow lumina in length of 3 cm. No tumor tissue was found and the whole biliary duct was sampled. The tissue samples were fixed in formalin, embedded in paraffin and routinely stained with hematoxylin and eosin stain. On microscope evaluation there was severe erosive chronic inflammation and fibrosis in the wall of the common bile duct. The sample from ampulla of Vater showed a luminal fungal structure with septate hyphae and acute angle branching, consistent with Aspergillus, surrounded by neutrophills (Figure 1). Additional histochemical stains were performed with Groccot silver methenamine (GSM) and PAS (Figure 2), Two weeks after the surgical procedure the patient is released (without the pathohistology report) in good condition with dietary advice protocols and check up in 1 month.
Discussion
Presentation of invasive aspergillosis as cholangitis although rare condition, has been described in the literature after biliary surgery, solid organ transplantation, in patient with acute leukemia and in patient with cholangiocarcinoma [3-6]. Our patient had no previous fungal infection, or pulmonary aspergillosis neither had liver damage or malignancy. Maggio RD et al. presented an isolated form of biliary aspergillosis in a patient with both kidney transplantation and a diffuse Large B-cell lymphoma which was diagnosed post-mortem. They point out the need for more sensitive diagnostic tests to detect early onset of this isolated form [7]. Our case also addresses the need for more specific tests or combination of procedures for early diagnosis and minimizing the risk of postoperative complications.
Laboratory analysis in cases with biliary aspergillosis showed increased levels of liver enzymes AST, ALT, and high ALP and GGT [8], as in our case. Serological tests of blood, urine or bronchoalveolar lavage are crucial in ongoing clinical studies for early diagnosis in invasive aspergillosis. Neutrophil recruitment has well established mechanisms in pulmonary aspergillosis regulated by epithelium-dependent IL1R/MyD88 signaling and inflammatory monocyte-mediated CARD9 signaling pathways [9]. It is unclear whether these are also responsible for other isolated forms of tissue inflammation. Our patient had no neutropenia but there were evident neutrophil accumulations around the hyphae accompanied with severe bile duct wall inflammation.
Understanding the pathogenesis is crucial for diagnosis of aspergillosis and also for the treatment taking in consideration the virulence of the pathogen, host environment and immune response. The guidelines for the treatment of different types of aspergillosis are published and should be implemented when needed [10]. The patient we present wasn’t suspected for aspergillosis and antifungal therapy was not applied.
We rule out the possibility of colonization during stenting due to the short period before surgery. The Aspergillus species are widely spread and the environment exposure is increased outside the health care units [11]. Hospital acquired aspergillosis should be prevented by antifungal prophylaxis. Conditions that mimic pancreatic cancer can have benign or malignant tumor morphology and can have even inflammatory etiology. Souza et al. present criptosporidiosis of biliary tract mimicking pancreatic cancer in patient with AIDS [12]. Our case is the first to our knowledge of aspergillosis of Ampulla of Vater with cholangitis that mimic pancreatic cancer.
Conclusion
In conclusion, cholangitis can mimic pancreatic cancer with obstructive jaundice and elevated liver enzymes and tumor markers. Biliary aspergillosis is a diagnostic challenge in a immunocompetent patients without neutropenia and without liver damage. Future studies should be conducted for early diagnosis and treatment of these rare aspergillosis presentations.
Conflict of interest: There are none.
Funding: This study received no funding.
Acknowledgements: None.
References
- A Zimmermann. Tumor-Like Lesions of the Hepatobiliary Tract Caused by Fungal Infections, in: Tumors and Tumor-Like Lesions of the Hepatobiliary Tract, Springer International Publishing, Cham, 2017.
- DW Warnock, RA Hajjeh, BA Lasker. Epidemiology and prevention of invasive aspergillosis, Curr. Infect. Dis. Rep. 2001; 3: 507- 516.
- BK Gupta, R Kumar, S Kaur, S Khurana. Incidence of fungal infection in extra hepatic biliary stone disease. Indian J. Pathol. Microbiol. 1993; 36: 110-112.
- C Yuchong, Z Dingheng, Y Zhizhong, Y Hongyu, H Jing, C Jianghan. Aspergillosis of Biliary Tract After Liver Transplantation: A Case Report, Mycopathologia. 2010; 170.
- JC García‐Ruiz, I Hernández, F Muñoz, A Alvarez‐Blanco, J Pontón, Cholangitis Due to Aspergillus fumigatus in a Patient with Acute Leukemia, Clin. Infect. Dis. 1998; 26.
- K Rothe, S Rasch, N Wantia, A Poszler, J Ulrich, C Schlag, W Huber, et al. Aspergillus fumigatus cholangitis in a patient with cholangiocarcinoma: case report and review of the literature, Infection. 2021; 49.
- R Di Maggio, G Calvaruso, D Renda, V Di Salvo, A Vulcano, B Bartolini, et al. AIsolated Aspergillosis of Biliary Tract in a Patient with Both Solid Organ Transplantation and Haematological Malignancy-A Case Report. 2020; 4.
- FM Yazar. A rare disease mimics postoperative bile leakage: Invasive Aspergillosis, Turkish J. Trauma Emerg. Surg. 2015.
- Latgé JP, Chamilos G. Aspergillus fumigatus and Aspergillosis in 2019. Clin Microbiol Rev. 2019; 33: e00140-18.
- Ullmann AJ, Aguado JM, Arikan-Akdagli S, Denning DW, Groll AH, Lagrou K, et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect. 2018; 24: e1-e38.
- Warnock DW, Hajjeh RA, Lasker BA. Epidemiology and Prevention of Invasive Aspergillosis. Curr Infect Dis Rep. 2001; 3:507- 516.
- Souza, Lenice do Rosário de et al. Cryptosporidiosis of the biliary tract mimicking pancreatic cancer in an AIDS patient. Revista da Sociedade Brasileira de Medicina Tropical. 2004; 37: 182-185.