Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 1
A metachronous metastatic carcinoma in colon interposition: The rare presentation of a rare pathology
Dzmitry Katovich1*; Heribert Ortlieb1; Claudia Grun1; Yolande Wandji Yimga1; Lothar Tietze2 ; Kai Neben1; Hans Weidenbach1
1 Klinikum Mittelbaden GgmbH, Baden-Baden, Germany.
2 Pathology Institut Ortenau Klinikum, Lahr, Germany.
*Corresponding Author : Dzmitry Katovich
Balgerstr. 50 76532, Baden-Baden Secretariat of
Pulmonology and Thoracic Surgery, Germany.
Email: 4kds86@gmail.com
Received : Nov 03, 2021
Accepted : Dec 13, 2021
Published : Dec 17, 2021
Archived : www.jjgastro.com
Copyright : © Katovich D (2021).
Abstract
A metachronous carcinoma in colon interposition after oesophagocoloplasty is a rare clinical situation. Fast all described cases were revealed by complains for dysphagia. In our case report we present a case of a patient with a solitary pulmonary nodule 10 years after oesophagus resection and colon interposition by oesophagus cancer.
Keywords: multiple cancer; video-assisted thoracic surgery (VATS); endoscopy
Citation: Dzmitry K, Heribert O, Claudia G, Yimga YW, Tietze L, et al. A metachronous metastatic carcinoma in colon interposition: the rare presentation of a rare pathology. Japanese J Gastroenterol Res. 2021; 1(9): 1045.
Introduction
Oesophagocoloplasty represents a useful technique to restore the intestinal continuity after oesophagus resection [1]. Metachronous malignancies in oesophagus cancer attract attention as a cause of survival rate decrease [2]. We present a case report of a metachronous colon cancer 10 years after oesophagocoloplasty by oesophagus squamous cell carcinoma with untypical clinical presentation.
Case description
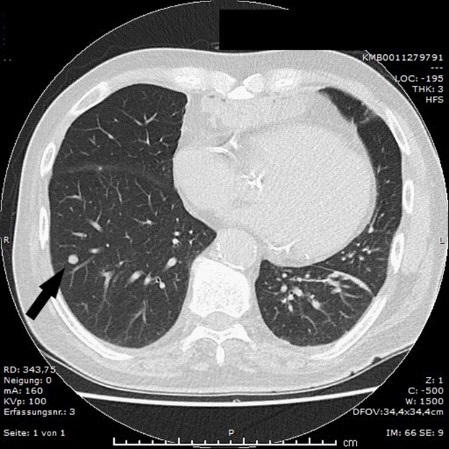
A 73 years old male patient was admitted to our thoracic department with the solitary pulmonary nodule in the lower right lobe (Figure 1).
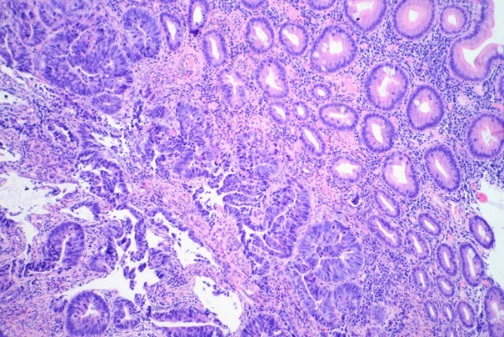
The nodule was revealed by the X-Ray examination because of the continuous cough and left chest pain. There were no dysphagia and any clinically significant laboratory changes. In anamnesis the oesophagocoloplasty for squamous cell carcinoma (SCC) of the oesophagus (pT2N1Mo) with adjuvant radio-chemotherapy was performed 10 years before. We performed videoassisted (VATS) wedge resection of the right lower lobe with the lesion. The pathology finding was colon type adenocarcinoma (Figure 2).
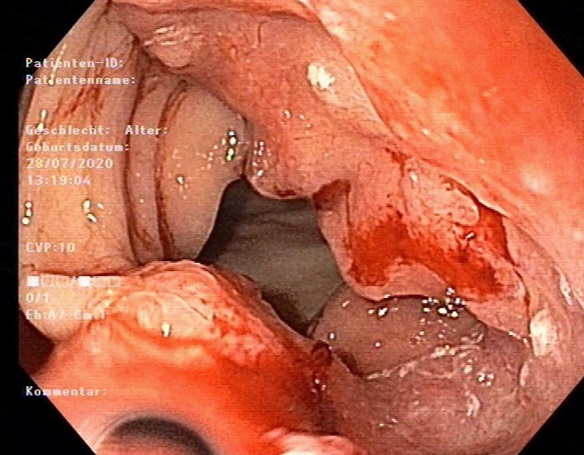
Because of tumour stage our multidisciplinary General Tumorboard advised the systemic treatment (Ardalan Protocol: 5-Floururacil 2600 mg/m² + Folinic acid 500 mg/m²). Before the chemotherapy initiation the patient was urgently admitted to the hospital because of atrial fibrillation episode and relevant 3-coronary arteries stenosis. The extra luminal percutaneous angioplasty was performed with 2 stents implantation. After the beginning of anticoagulant therapy the patient had an episode of gastrointestinal bleeding from the colon interportal, that required no surgical or endoscopic treatment. We could start the chemotherapy 10 weeks after the diagnostic VATS with a normal patient‘s tolerance. At the time of article writing the patient is clinically stable after 6 full cycles of chemotherapy, has no dysphagia and stable body weight. Actual computer tomogra . Actual computer tomography and EGDS control revealed no signs of tumour progression.
Discussion
Metachronous colorectal carcinoma (MCC) in a colon interposition after oesophagocoloplasty is a rare pathology. The lite analysis showed 23 cases from 1968 to 2019, where oesophagocoloplasties were performed for benign oesophagus stenosis. We could find only 12 pure MCCs [3-5] previously operated on oesophagus cancer. Oesophagus and colorectal neoplasms share some risk factors and patients with SCC of the oesophagus have increased risk of colorectal cancer [2,6]. The long-standing colonic mucosa irritation by gastric juice and bile was also described as a risk factor [1,7]. Fast all reported cases of patients with MCC in a colon interposition after esophagocoloplasty reported dysphagia and weight loss as a clinical manifestation. In our case report there were no clinical signs of lumen obstruction, but the solitary metastatic nodule in the right lung was found. To our opinion, the clinical presentation in this particular case with cough and left chest pain could be explained rather by coronary artery disease and gastroesophageal reflux than by small solitary pulmonary nodule in the right lower lobe. In our case report the tumour was found 10 years after initial esophagus cancer, what corresponds to literature data with median 8,5 years. As a limitation of our case report we had no information whether a colonoscopy was performed before the oesophagocoloplasty. But in considering the interval between the presentation of two tumour cases it could be not relevant for this particular patient.
Conclusion
For our knowledge, this is the first presentation of initial asymptomatic metastatic spread of a metachronous colon carcinoma in a colon interposition after oesophagocoloplasty. Despite the absence of standard protocol regular endoscopic and thorax-abdomen CT-control for patients after oesophagus, cancer surgical treatment with colon interposition could be advised.
References
- Aurello P, Petrucciani N, Sirimarco D, Mangogna LM, Nigri G, Valabrega S, et al. Esophagectomy with Esophagocoloplasty for Malignancies: Indications, Technique (with Video), and Results. Systematic Review of the Literature. J Gastrointest Surg. 2017; 21: 1557-61.
- Jang BI, Hwang MJ. Do esophageal squamous cell carcinoma patients have an increased risk of coexisting colorectal neoplasms? Gut Liver. 2016; 10: 6-7.
- De Moura D, Ribeiro I, Coronel M, De Moura E, Carvalho J, Baba E, et al. Primary adenocarcinoma arising in esophageal colon interposition for corrosive esophageal injury: a case report and review of the literature. Endosc Int Open. 2018; 06: E1406-9.
- Simões C, Moura M, Noronha Ferreira C, Rosa R, Freire JP, Carrilho Ribeiro L, et al. Lateral Spreading Tumor Arising in an Interposed Colonic Segment. ACG Case Reports J. 2019; 6: e00245.
- Sohn M, Agha A, Trum S, Moser C, Gundling F, Hochrein A, et al. Frequency of polyps and adenocarcinoma in colon interposition after esophagectomy in adulthood – A systematic review. Anticancer Res. 2019; 39: 6419-30.
- Baeg MK, Choi MG, Jung YD, Ko SH, Lim CH, Kim HH, et al. Esophageal squamous cell carcinoma patients have an increased risk of coexisting colorectal neoplasms. Gut Liver. 2016; 10:76- 82.
- Grunner S, Gilshtein H, Kakiashvili E, Kluger Y. Adenocarcinoma in colonic interposition. Case Rep Oncol. 2013; 6:186-8.