Japanese Journal of Gastroenterology Research
Review Article - Open Access, Volume 1
Origin and properties of hepatocellular carcinoma cell lines
Lakshana D Puttahanumantharayappa; Nirmala G Sannappa Gowda; Varsha D Shiragannavar; Prasanna K Santhekadur*
Department of Biochemistry, Center of Excellence in Molecular Biology & Regenerative Medicine, JSS Medical College, JSS Academy of Higher Education and Research, Mysore, Karnataka, India.
*Corresponding Author: Prasanna K Santhekadur
Associate Professor, Department of Biochemistry, Center of Excellence in Molecular Biology and Regenerative Medicine, JSS Medical College, JSS Academy of Higher Education and Research, Sri Shivarathreeshwara Nagar, Mysore-570015, Karnataka, India.
Tel: 646-962-4000,
Tel: +91-91086 55013;<
Email: prasannakumars@jssuni.edu.in
Received : Oct 30, 2021
Accepted : Nov 26, 2021
Published : Dec 01, 2021
Archived : www.jjgastro.com
Copyright : © Santhekadur PK (2021).
Abstract
The liver is one of the vital organs in human beings. It is responsible for several functions such as energy homeostasis, detoxification, regulating blood sugar levels, protein synthesis, bile acid secretion, cholesterol production and glycogen storage. Hepatocellular Carcinoma (HCC) alternately referred to as malignant hepatoma accounts to ~75% of all liver cancers and its resistance to therapeutics at progressed stages makes it lethal. Some of the main causes of HCC include HBV, HCV, aflatoxin, chronic alcoholism, excess nutrition, liver cirrhosis, iron over load, Wilson's disease, and type 2 diabetes. It is essential to detect the underlying causes of HCC at the cellular and molecular levels to develop drugs and find a potential cure for the disease. Several ongoing studies on HCC cell lines help to understand the gene expressions, multiple signaling pathways and differential drug responses to HCC. This review article provides insights to the possible molecular pathways involved in the origin of commonly used HCC cell lines and the signals that are functionally active in them.
Keywords: hepatocellular carcinoma; malignant; cell lines; molecular pathways; Msignals.
Abbreviations: HCC: Hepatocellular Carcinoma; NAFLD: Nonalcoholic Fatty Liver Disease; HBV: Hepatitis B Virus; HCV: Hepatitis C Virus; CDK1: Cyclin-Dependent Kinase 1; C-Myc: Cellular Myelocytomatosis Oncogene; AEG-1: Astrocyte Elevated Gene-1; SND1: Staphylococcal Nuclease And Tudor Domain Containing 1; LSF: Late SV40 Factor; TGF-Β: Transforming Growth Factor-Β; ERK: Extracellular Signal-Regulated Kinase; MEK: Mitogen-Activated Protein Kinase; PI3K: Phosphoinositide 3-Kinases; Mtor: Mammalian Target Of Rapamycin; NF-Κb: Nuclear Factor Kappa-Light-Chain-Enhancer Of Activated B Cells; SHH: Sonic Hedgehog; TIMP: Tissue Inhibitor Of Metalloproteinase; PTEN: Phosphatase And Tensin Homolog; MMP: Matrix Metalloprotease; CD24: Cluster Of Differentiation 24; Epcam: Epithelial Cellular Adhesion Molecule; BM-MSC: Bone Marrow Derived Mesenchymal Stem Cells; TNF: Tumor Necrosis Factor; IGF: Insulin-Like Growth Factor.
Citation: Puttahanumantharayappa LD, Sannappa Gowda NG, Shiragannavar VD, Prasanna K Santhekadur. Origin and properties of hepatocellular carcinoma cell lines. Japanese J Gastroenterol Res. 2021; 1(8): 1040.
Introduction
Liver cancer or HCC is rapidly arising as a health priority accounting for a significant number of cancer-related deaths globally [1-5]. HCC is a common malignancy and can be fatal due to a lack of remedies for progressed stages of tumor [6]. To develop a potential curative for advanced HCC, it is essential to understand the underlying causes and features of HCC [7-9]. Although several reports associate the contribution of natural carcinogens such as aflatoxin to HCC, HBV and HCV plays a vital role [7,9,11]. At molecular level, the viral infection advances by associating with the p53 gene. This gene is tumor suppressor and obstructs CDK1 or p21 [8,9,12]. Carcinogens like aflatoxin, promote mutation in tumor suppressor genes and evidence supports the role of proto-oncogenes in HCC [10]. Few principles oncogenes such as c-Myc (Cellular myelocytomatosis oncogene), AEG-1 (Astrocyte elevated gene-1), Staphylococcal Nuclease and Tudor Domain Containing 1 (p100, Tudor SN, SND1) and LSF (Late SV40 factor) are up regulated in HCC. Several signaling pathway like the TGF-β, ERK, MEK, PI3K/Akt/mTOR and NF-κB are active in HCC and activated signaling pathways differ based on cell lines [12,13,9,14-16]. It is required to carry out in vitro analysis to examine the individual signaling pathways in distinct cell lines. Some of the routinely analyzed cell lines are Hep3B, HepG2, Huh7, Sk-Hep1, QGY-7703, PLC/PRF/5 (Alexander) and immortalized THLE-2 and THLE-3 as listed in (Table 1). The establishment and characterization of cell lines from various sources has paved way to the present understanding of HCC at the molecular level. However, it is essential to construct a systematic study of these cell lines based on their origin and molecular pathways to understand the drug-resistant mechanisms in HCC and develop novel medications.
Table 1: Origin and properties of commonly used HCC cell lines.
| Name | Origin and ethnicity | Year | Morphology | Growth properties | Comments |
|---|---|---|---|---|---|
| Hep3B | 8-year-old black male | 1976 | Epithelial | Adherent | Presence of HBV genome |
| HepG2 | 15-year-old Caucasian Argentinean male | 1975 | Epithelial | Adherent | No evidence of HBV geneome |
| Huh-7 | 57-year-old Japanese male | 1982 | Epithelial | Adherent | Negative for HCV |
| THLE-2 & THLE-3 | Primary normal liver cells | 1990 | Epithelial | Adherent | Cells are infected with SV40 large T antigen |
| Sk-Hep-1 | 52-year-old Caucasian male | 1971 | Endothelial | Adherent | Absence of endothelial markers |
| QGY-7703 | 35-year-old Chinese female | 1981 | Epithelial-Mesenchymal transition | Adherent | Aflatoxin induced HCC |
| PLC/PRF/5 (Alexander) | 24-year-old Shangaan male (Africa) | 1975 | Epithelial | Adherent | Presence of HBsAg |
| SNU-423 | 40-year-old Korean male | 1990 | Epithelial | Adherent | HBV DNA detected |
| FOCUS | 60-year-old male | 1985 | Fibroblast | Adherent | Positive for HBV |
HCC cell lines
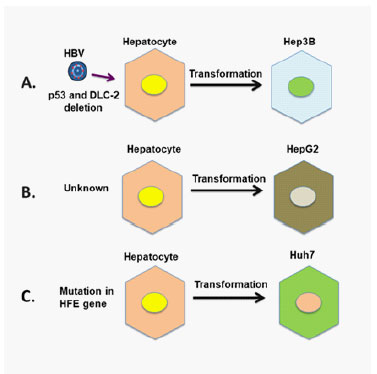
Hep3B
Hep3B cell lines were initially established by Aden et al. [17]. It was isolated at Barbara B. Knowles lab, Wistar Institute, Philadelphia, USA. The cell line was sourced from hepatic biopsies of a young black male. Aged 8, he was a victim of primary liver carcinoma (Figure 1A). The cell line contains an integrated HBV genome and produces two primary polypeptides of HBV surface antigen (HBsAg) [18]. Several genes like MMP-9 (matrix metalloproteinase) [19], Survivin [20], TGF-β (transforming growth factor) [21] and SHH (sonic hedgehog) [22] are expressed in Hep3B. Genes like plasminogen [23], TIMP-1 and TIMP-3 (tissue inhibitors of metalloproteinases) are suppressed. PTEN tumor suppressor protein in expressed and pathways like ERK and NF-κB is active. Studies established the absence of tumor suppressor gene p53 [24] and the expression of transcription factor NF-κB is detected [25]. The doubling time of Hep3B is ~36 hours.
HepG2
The HepG2 cell line was also isolated at Barbara B. Knowles lab, Wistar Institute, Philadelphia, USA (Figure 1B). It is a human hepatoma obtained from liver tumor biopsies of a 15-year-old Caucasian Argentinean male [17]. These cell lines are epithelial like and non-tumorigenic with large multiplication rate [26]. Studies have reported that HepG2 is p53 wild type. Expression of genes like Cyclin D1, TGF-β type I receptor, TIMP-1 and TIMP-3 is up regulated, while there is a decline in the expression of TGF-β, SHH and MMP-9 [27]. A proteome profiling revealed that HepG2 retained hepatocytes like features [28]. A significant number of plasma proteins like albumin, transferrin, plasminogen, characteristic of hepatocytes are present in the cell line and pathways like ERK and NF-ҡB is active as well. The doubling time of HepG2 is ~48 hours [29].
Huh7
Huh 7 and its derivatives have its origin from the human hepatoma. This cell line was established in 1982 by Nakabayshi et al., [30]. It was sourced from a Japanese man, aged 57. Huh7 is an excellent substitute for primary hepatocytes and a suitable host for in vitro propagation of HCV. It is immortal, epithelial like and tumorigenic (Figure 1C). Huh-7 produces the following human plasma proteins like albumin, fibrinogen, transferrin, lipoprotein etc. Besides it also secretes anti-carcinoembryonic antigen reactive proteins. Flow cytometry study of Huh-7 cells ascertained the expression of CD24 (cluster of differentiation 24), prominin-1 and EpCAM (epithelial cellular adhesion molecule) genes. The p53 gene in Huh-7 cells with mutations at codon 249 and 220 respectively, has a prolonged half-life thus, accumulating in the nuclei [24]. ERK and NF-ҡB pathways are active. Doubling time of Huh-7 is ~24 hours.
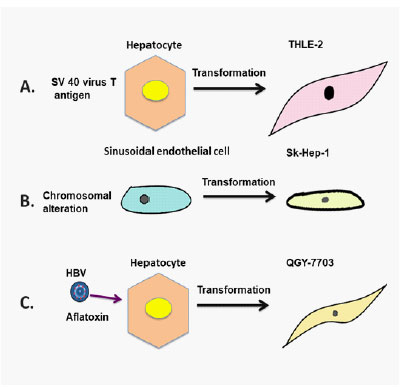
THLE-2 and THLE-3
The immortalized cell lines THLE-2 and THLE-3 are human hepatocytes. They are derived by introducing SV-40 large T-antigen gene (Figure 2A). A retroviral vector containing the Bgl I-Hpa I segment of the gene is packed into PA317 (packing cells) to develop the virus [31]. Both THLE-2 and THLE-3 have features of typical mature hepatic epithelial cells. These cell lines are non-tumorigenic with a doubling time of ~40 hours. Almost all signaling pathways are active in these cell lines and they expressed cytokeratin 18, albumin and cytokeratin 19 [31]. Carcinogenic metabolites are produced through functional cytochrome p450 pathway. Enzymes like glutathione S-transferases and glutathione peroxidase are held on to by the cell lines to metabolize chemical carcinogens [32].
Sk-Hep-1
Sk-Hep-1 is a continuing cell line. It was procured from the ascites fluids of a 52-year-old Caucasian male with hepatic carcinoma (Figure 2B). This cell line is tumorigenic with endothelial origin [33]. Although SK-HEP-1 serves as a model for HCC, it is different in terms of protein and gene expression [34]. The cells are able to transform into osteoblasts, adipocytes and mesenchymal stem cells acquired from the bone marrow (BM-MSC). This cell line expressed almost all MSC markers but did not express any hepato specific genes including fibrinogen, albumin and alpha fetoprotein. ERK and NF-ҡB pathways are active in Sk-Hep1. Despite its endothelial origin, the endothelial markers were undetected in the cell line [35]. Doubling time of Sk-Hep-1 is ~30 hours.
QGY-7703
The QGY-7703 was isolated in Shanghai Institute of Cell Biology, China. This cell line was obtained from primary HCC of 35 years old female patient belonging to Qidong region which has the highest morbidity rate of HCC in China (Figure 2C). Studies have reported that aflatoxin exposure and HBV infection as interactive risk factors for primary liver cancer in this region [36]. QGY-7703 demonstrates characteristics and expresses IGF-II (insulin like growth factor) [37]. Two proteins acyl-protein thioesterase 2 and 17-beta-hydroxysteroid dehydrogenase 10 expressed in QGY-7703 are vital for tumor development. ERK and NF-ĸB pathways are active in QGY-7703.During apoptosis, TGF-beta, TNF, FAS, p38MAPK, and p53 signaling pathways are active in the cell line but there is no expression of E-cadherin. The doubling time for QGY-7703 is ~20 hours.
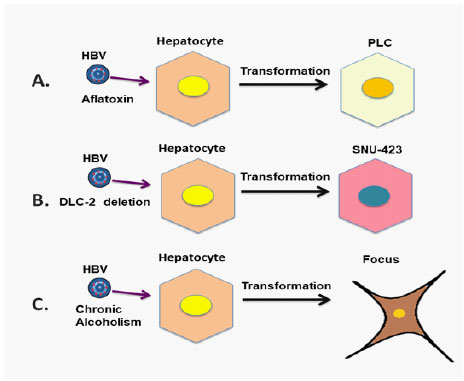
PLC/PRF/5(Alexander)
Dr. J. J. Alexander established the Alexander or PLC/PRF/5 cell line in Johannesburg, South Africa. It was sourced from a 24 years Shangaan male with HCC from Mozambique (Figure 3A). This cell line continuously produces the HBsAg, however there was no expression for other markers of HBV synthesis [38]. Some oncogenes like c-Myc, c-abl, c-ha-ras c-fes, c-fms, and c-sis oncogenes are indicated in the cell line along with HBsAg. The ERK, TGF-β, NF-κB, Akt/mTOR pathways are active and p53 gene mutation is indicated. Doubling time of this cell line is 30-40 hours.
SNU-423
The cell line SNU-423 (Seoul National University-423) was established by J.G. Park and et al. It was derived from primary hepatocellular carcinoma taken from a Korean male (Figure 3B). The cultured cells are multinucleated and HBV DNA was detected. SNU cells shows loss of normal functioning of p53 gene [39]. The cell lines are generally used to examine the expression of HBV and IGF. The ERK, TGF-β, NF-κB and Akt/mTOR pathways are active in this cell line. SNU-423 has a doubling time of 72 hours.
Focus
FOCUS (Friendship of China and United States) cell line originates from human HCC. It was obtained from a male patient aged 63 who had a history of yellow jaundice and chronic alcoholism (Figure 3C). Transcripts of p53 were not detected while there is expression of DLC-2 gene in FOCUS. This cell line is positive for HBV and expresses alpha-fetoprotein, fibrinogen, alpha 1-antitrypsin and CEA. Activities of aspartate aminotransferase and glucose-6-phosphatase are detected in FOCUS [40]. ERK, TGF-β, NF-κB and Akt/mTOR pathways are active. The cell line lacks Alpha-Fetoprotein and EMT markers. Doubling time of the cell line is 42 - 48 hours.
Conclusion
HCC is a complex health condition caused due to several factors like excess nutrition, exposure to toxins, alcoholism, HBV and HCV. Recent surge in the number of HCC cases due to diabetes, obesity and fatty liver diseases has increased the necessity for developing new drugs. Screening of various drugs in vivo along with in vitro studies has contributed to several drug discoveries. Laborious maintenance of animal models can be overcome by a cell line-based system to identify novel markers of HCC for improved diagnosis. Due to their immortality, HCC cell lines provide a provision for easy handling and they resemble the original tumor from which they were established. Over the last few decades various HCC cell lines were established from multiple ethnic groups all over the world and developed as stated in (Table 1). They are exploited for drugs screening, examining cell signaling pathways and to understand gene expression profiles associated with the HCC. The effects of drug like taxol and 5-Flurouracil on QGY-7703 have already been elucidated. Studies have also examined the response of HepG-2 and Huh-7 towards therapeutic agents like curcumin. Doxorubicin and Sorafenib are used to examine the properties of Hep3B, HepG2, PLC-PRF-5 and SK-Hep. In summary, this review helps in further understanding of various HCC cell lines, based on their origin and background. It highlights the behavior of cell lines along with mutations of genes and alterations in signaling pathways.
Declarations
Acknowledgements: Dr Prasanna K. Santhekadur thanks DBT-India for awarding the prestigious Ramalingaswami Fellowship. Miss Lakshana D. Puttahanumantharayappa extends gratitude to JSS Medical College and JSS AHER for the research opportunity.
References
- Ferenci P, Fried M, Labrecque D, Bruix J, Sherman M, Omata M, et al. World Gastroenterology Organization Hepatocellular carcinoma (HCC): a global perspective. J Clin Gastroenterol. 2010; 44: 239-245.
- Parkin DM, Bray F, Ferlay J and Pisani P. Global cancer statistics 2002. CA Cancer J Clin 2005; 55: 74-108.
- El Serag HB and Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med 1999; 340: 745-750.
- Sherman M. Hepatocellular carcinoma: epidemiology, risk factors, and screening. Semin Liver Dis 2005; 25: 143-154.
- Llove JM and Bruix. J. Molecular targeted therapies in hepatocellular carcinoma. Hepatology. 2008; 48: 1312-27.
- Chuma M, Terashita K and Sakamoto N. New molecularly targeted therapies against advanced hepatocellular carcinoma: from molecular pathogenesis to clinical trials and future directions. Hepatol Res. 2015; 45: E1-E11.
- Brechot C, Pourcel C, Louise A, Rain, B and Tiollais P. Presence of integrated hepatitis B virus DNA sequences in cellular DNA of human hepatocellular carcinoma. Nature. 1980; 286: 533-535.
- Kwun, H.J., Jung, E.Y., Ahn, J.Y., Lee, M.N., and Jang, K.L. 2001. p53-dependent transcriptional repression of p21(waf1) by hepatitis C virus NS3. J Gen Virol. 2001; 82: 2235-2241.
- Yoo BK, Emdad L, Su ZZ, Villanueva A, Chiang DY, Mukhopadhyay ND, et al. Astrocyte elevated gene-1 regulates hepatocellular carcinoma development and progression. J Clin Invest. 2009; 119: 465-477.
- Hoshida Y, Fuchs BC and Tanabe KK. Prevention of hepatocellular carcinoma: Potential targets, experimental models, and clinical challenges. Curr Cancer Drug Targets. 2012; 12: 1129-1159.
- Feitelson MA, and Duan LX. Hepatitis B virus X antigen in the pathogenesis of chronic infections and the development of hepatocellular carcinoma. Am J Pathol. 1994; 150: 1141–1157.
- Lee MN, Jung EY, Kwun HJ, Jun HK, Yu DY, Choi YH, et al. Hepatitis C virus core protein represses the p21 promoter through inhibition of a TGF-beta pathway. J Gen Virol. 2002; 83: 2145-2151.
- Abou-Elella A, Gramlich T, Fritsch C and Gansler T. c-myc amplification in hepatocellular carcinoma predicts unfavorable prognosis. Mod Pathol. 1996; 9: 95-98.
- Yoo BK, Santhekadur PK, Gredler R, Chen D, Emdad L, Bhutia S, et al. Increased RNA-induced silencing complex (RISC) activity contributes to hepatocellular carcinoma. Hepatology. 2011; 53: 1538-1548.
- Yoo BK, Emdad L, Gredler R, Fuller C, Dumur CI, Jones KH, et al. Transcription factor Late SV40 Factor (LSF) functions as an oncogene in hepatocellular carcinoma. Proc Natl Acad Sci U S A. 2010; 107: 8357-8362.
- Santhekadur PK, Akiel M, Emdad L, Gredler R, Srivastava J, Rajasekaran D, et al. Staphylococcal nuclease domain containing-1 (SND1) promotes migration and invasion via angiotensin II type 1 receptor (AT1R) and TGFβ signaling. FEBS Open Bio. 2014; 4: 353-361.
- Aden DP, Fogel A, Plotkin S, Damjanov I and Knowles BB. Controlled synthesis of HBsAg in a differentiated human liver carcinoma-derived cell line. Nature. 1979; 282: 615–616.
- Knowles BB, Howe CC and Aden DP. Human hepatocellular carcinoma cell lines secrete the major plasma proteins and hepatitis B surface antigen. Science. 1980; 209: 497-499.
- Chung TW, Lee Y and Kim CH. Hepatitis B viral HBx induces matrix metalloproteinase-9 gene expression through activation of ERK and PI-3 K/AKT pathways: involvement of invasive potential. FASEB J. 2004; 18 1123–1125.
- Kusaba M, Nakao K, Goto T, Nishimura D, Kawashimo H, Shibata H, et al. Abrogation of constitutive STAT3 activity sensitizes human hepatoma cells to TRAIL-mediated apoptosis. J Hepatol. 2007; 47: 546-555.
- Liu P, Menon K, Alvarez E, Lu K and Teicher BA. Transforming growth factor-beta and response to anticancer therapies in human liver and gastric tumors in vitro and in vivo. Int J Oncol.2000; 16: 599–610.
- Huang S, He J, Zhang X, Bian Y, Yang L, Xie G, et al. Activation of the hedgehog pathway in human hepatocellular carcinomas. Carcinogenesis. 2006; 27: 1334-1340.
- Malgaretti N, Bruno L, Pontoglio M, Candiani G, Meroni G, Ottolenghi S, et al. Definition of the transcription initiation site of human plasminogen gene in liver and non hepatic cell lines. Biochem Biophys Res Commun. 1990; 173: 1013–1018.
- Bressac B, Galvin KM, Liang TJ, Isselbacher KJ, Wands JR and Ozturk M. Abnormal structure and expression of p53 gene in human hepatocellular carcinoma. Proc Natl Acad Sci U S A. 1990; 87: 1973-1977.
- Chiao PJ, Na R, Niu J, Sclabas GM, Dong Q and Curley SA. Role of Rel/NF-kappaB transcription factors in apoptosis of human hepatocellular carcinoma cells. Cancer. 2002; 95: 1696-1705.
- Donato MT, Tolosa L and Gómez-Lechón MJ. Culture and functional characterization of human hepatoma HepG2 cells. Methods Mol Biol. 2015; 1250: 77-93.
- Qiu GH, Xie X, Xu F, Shi X, Wang Y and Deng L. Distinctive pharmacological differences between liver cancer cell lines HepG2 and Hep3B. Cytotechnology. 2015; 67 :1-12.
- Slany A, Haudek VJ, Zwickl H, Gundacker NC, Grusch M, Weiss TS, et al. Cell characterization by proteome profiling applied to primary hepatocytes and hepatocyte cell lines Hep-G2 and Hep-3B. J Proteome Res. 2010; 9: 6–21.
- Norouzzadeh M, Kalikias Y, Mohamadpur Z, Sharifi L and Mahmoudi M. Determining population doubling time and the appropriate number of HepG2 cells for culturing in 6-well plate. Int Res Bas Sci. 2016.
- Nakabayashi H, Taketa K, Miyano K, Yamane T and Sato J. Growth of human hepatoma cell lines with differentiated functions in chemically defined medium. Cancer Res. 1982; 42: 3858-3863.
- Pfeifer AM, Cole KE, Smoot DT, Weston A, Groopman JD, Shields PG, et al. Simian virus 40 large tumor antigen-immortalized normal human liver epithelial cells express hepatocyte characteristics and metabolize chemical carcinogens. Proc Natl Acad Sci U S A. 1993; 90: 5123-5127.
- Yeşiltepe O, Güler Çelik E, Geyik C, Gümüş ZP, Odaci Demirkol D, Coşkunol H, Timur S. Preparation of glutathione loaded nanoemulsions and testing of hepatoprotective activity on THLE-2 cells. Turk J Chem. 2021; 45:436-451.
- Heffelfinger SC, Hawkins HH, Barrish J, Taylor L and Darlington GJ. SK HEP-1: a human cell line of endothelial origin. In Vitro Cellular & Dev Biol. 1992; 28: 136-142.
- Tai Y, Gao JH, Zhao C, Tong H, Zheng SP, Huang ZY, et al. SK-Hep1: not hepatocellular carcinoma cells but a cell model for liver sinusoidal endothelial cells. Int J Clin Exp Pathol. 2018; 11: 2931-2938.
- Eun JR, Jung YJ, Zhang Y, Zhang Y, Tschudy-Seney B, Ramsamooj R, et al. Hepatoma SK Hep-1 cells exhibit characteristics of oncogenic mesenchymal stem cells with highly metastatic capacity. PLoS One. 2014; 9: e110744.
- Qian GS, Ross RK, Yu MC, Yuan JM, Gao YT, Henderson BE, et al. A follow-up study of urinary markers of aflatoxin exposure and liver cancer risk in Shanghai, People's Republic of China. Cancer Epidemiol Biomarkers Prev. 1994; 3: 3–10.
- Su Q, Liu YF, Zhang JF, Zhang SX, Li DF and Yang JJ. Expression of insulin‐like growth factor II in hepatitis B, cirrhosis and hepatocellular carcinoma: its relationship with hepatitis B virus antigen expression. Hepatology. 1994; 20: 788-799.
- Daemer RJ, Feinstone SM, Alexander JJ, Tully JG, London WT, Wong DC, et al. PLC/PRF/5 (Alexander) hepatoma cell line: further characterization and studies of infectivity. Infect Immun. 1980; 30: 607-611.
- Ku JL and Park JG. Biology of SNU cell lines. Cancer Res Treat. 2005; 37: 1-19.
- He L, Isselbacher KJ, Wands JR, Goodman HM, Shih C and Quaroni A. Establishment and characterization of a new human hepatocellular carcinoma cell line. In vitro. 1984; 20: 493-504.