Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 1
An unusual case of massive GI bleeding in an immunosuppressed patient
J Samuel Lagos1; Amit Mehta2; David Wan2*
1San Fernando School of Medicine, Universidad Nacional Mayor de San Marcos, Lima, Peru.
2New York-Presbyterian Weill Cornell Medical Center, New York, NY, USA.
*Corresponding Author: David Wan
Division of Gastroenterology and Hepatology, Weill Cornell Medicine 1283 York Ave, 9th Floor New York, NY 10065, USA.
Tel: 646-962-4000,
Fax: 646-962-0110;
Email: daw9044@med.cornell.edu
Received : Oct 29, 2021
Accepted : Nov 25, 2021
Published : Nov 30, 2021
Archived : www.jjgastro.com
Copyright : © Wan D (2021).
Abstract
Nematode hyperinfection classically presents with eosinophilia; however, immunosuppressed patients on corticosteroid therapy or with chronic HTLV 1-2 infection do not necessarily express this eosinophilic pattern. We present a patient with T cell lymphoma and HTLV 1-2 infection with massive GI bleeding that illustrates this atypical scenario. Concomitant pyogenic infection and/or steroid administration can blunt the eosinophilia response in Strongyloides infections, and it is important to rule out the infection in a patient from an endemic area.
Keywords: strongyloides infection; HTLV; GI bleeding.
Citation: Lagos JS, Mehta A, Wan D. An unusual case of massive GI bleeding in an immunosuppressed patient. Japanese J Gastroenterol Res. 2021; 1(8): 1039.
Introduction
Strongyloides stercolaris infection is a disease found worldwide; however, its incidence is highest in developing countries. The parasite is most commonly acquired through skin contact with contaminated soil. Individuals infected with Strongyloides usually present with variable grades of eosinophilia. However, there are some cases where this pattern is masked.
Case Report
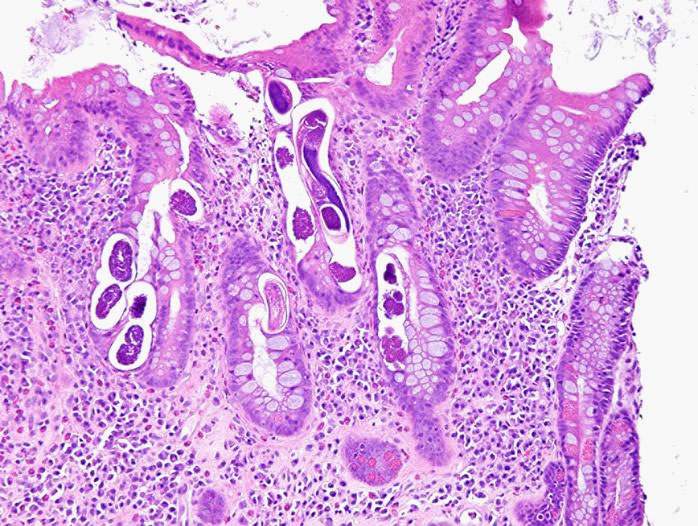
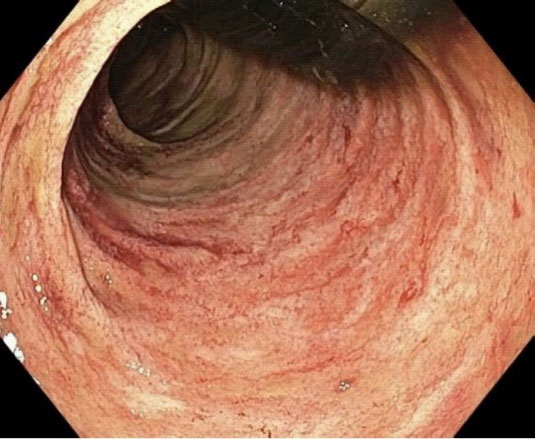
A 60 year old male with a recent diagnosis of C. difficile colitis was admitted to the emergency department with syncope and failure to thrive. His past medical history was notable for chronic inactive hepatitis B, peripheral T cell lymphoma on azacitidine and cyclophosphamide, doxorubicin, vincristine, and prednisone, and chronic HLTV 1-2. The patient reported 6 days of nausea, vomiting and watery diarrhea occurring approximately 2-3 times daily, with associated petechial rash over his torso as well as all four limbs. On examination he was found to be tachycardic and hypovolemic which responded well to fluid resuscitation. Physical examination was notable for a bilateral petechial rash on his legs, arms, and torso, the rest of the examination was unremarkable. His labs were notable for hemoglobin of 11.3 g/dL, normal white blood cell count, but with 90% neutrophilia, ALT 135 U/L, total bilirubin of 6.8 mg/dL, direct bilirubin of 5.6 mg/dL, and alkaline phosphatase of 221 U/L, and albumin of 1.6 g/dL. Abdominal US revealed gallbladder sludge and common bile duct of 9 mm, but MRCP did not show any choledocholithiasis or biliary dilation. On hospital day four, the patient acutely developed melena, hematochezia, hemodynamic instability, and hemoglobin nadir to 5.5 g/dL packed red cell transfusions requiring emergent EGD and flexible sigmoidoscopy showing diffuse mucosal oozing in the upper and lower GI tracts with ulcers with a moth-eaten appearance (Figure 1). Biopsies were taken.
Discussion
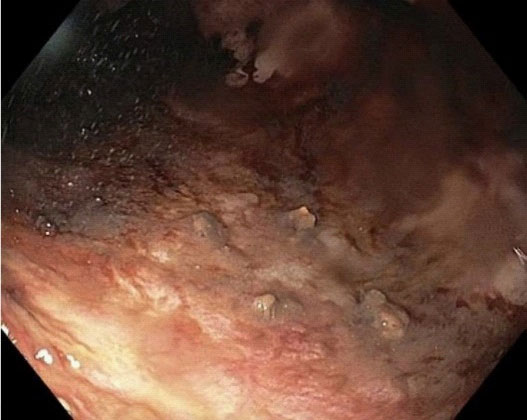
The pathology revealed worms suggestive of Strongyloides (see Figure 2). Upon further questioning, the patient was born in the Dominican Republic and moved to the United States more than 10 years ago but he denied history of recent travel. The patient was started on ivermectin which was then switched to praziquantel given concern of inadequate absorption due to ileus. The patient clinically improved with cessation of bleeding. A subsequent ERCP was performed to rule out biliary obstruction which was normal, and his liver chemistries significantly improved. He was discharged to complete a 14-day course of praziquantel from his first negative ova and parasite stool exam.
Strongyloides hyperinfection syndrome (SHS) has been defined as an overproliferation of strongyloides in the lungs or bowels that is caused by an autoinfection process [1]. It is associated with immunosuppressed patients on chemotherapy, steroid therapy, underlying malignancy or chronic HTLV1-2 infection where the T cell mediated responded is altered. Patients with SHS usually present with symptoms similar to classic infection like diarrhea, nausea, vomiting, and weight loss. However, due to increased parasite turnaround and dissemination, patients with hyperinfection syndrome and disseminated disease often have catastrophic clinical manifestations such as shock, disseminated intravascular coagulation, meningitis, renal failure, and/or respiratory failure. This patient had many presenting symptoms, but the development of massive GI bleeding and abnormal liver chemistries is rare [2].
Strongyloides infections usually present with variable grades of eosinophilia. Eosinophilia, however, may be suppressed or absent in disseminated disease because of concomitant pyogenic infection or steroid administration as we can see in this patient. Additionally, patients with HTLV-1 infection express high levels of interferon-gamma production, which decreases the production of interleukin (IL)-4, IL-5, IL-13, and IgE, important molecules in host defense against Strongyloides [3]. As a consequence, both factors could have contributed to the absence of eosinophilia in this patient.
Strongyloides colitis can sometimes mimic ulcerative colitis, but distinctive features of the strongyloidiasis include skip pattern of the inflammation, distal attenuation of the disease, eosinophil-rich infiltrates, relatively intact crypt architecture, and frequent involvement of submucosa [5].
One should suspect a strongyloides infection when a patient comes from an endemic area. It is recommended to screen for latent infections or to treat the patient empirically prior to the initiation of immunosuppressive therapy.
References
- Fardet L, Généreau T, Poirot JL, Guidet B, Kettaneh A, Cabane J. Severe strongyloidiasis in corticosteroid-treated patients: case series and literature review. J Infect. 2007; 54: 18-27.
- Csermely L, Jaafar H, Kristensen J, Castella A, Gorka W, Chebli AA, Trab F, Alizadeh H, Hunyady B. Strongyloides hyper-infection causing life-threatening gastrointestinal bleeding. World J Gastroenterol. 2006; 12: 6401-4.
- Carvalho EM, Da Fonseca Porto A. Epidemiological and clinical interaction between HTLV-1 and Strongyloides stercoralis. Parasite Immunol. 2004; 26: 487.
- Qu Z, Kundu UR, Abadeer RA, Wanger A. Strongyloides colitis is a lethal mimic of ulcerative colitis: the key morphologic differential diagnosis. Hum Pathol. 2009; 40: 572.