Japanese Journal of Gastroenterology Research
Research Article - Open Access, Volume 1
Health coaching experience in Minerbio (Italy): Global impact on weight, BMI, waist circumference and blood pressure
Plazzi Andrea, Di Fine Maria, Giulia Roda; Enrico Roda*
FISS, Fondazione Istituto di Scienze della Salute, Bologna, Italy.
*Corresponding Author: Enrico Roda
FISS, Fondazione Istituto di Scienze della Salute, Bologna, Italy.
Email: segreteria@profenricoroda.it
Received : Sep 24, 2021
Accepted : Nov 17, 2021
Published : Nov 23, 2021
Archived : www.jjgastro.com
Copyright : © Roda E (2021).
Abstract
In the last decade, growing evidence have shown the cardioprotective role of the Mediterranean diet. Health coaching has a pivotal role in primary care, helping patients to self-education concerning diet and physical activity.
Our study is a one-year health coaching pilot study with the aim to instruct patients' lifestyle to a Mediterranean diet and exercises to reduce cardiovascular disease risks, diabetes, and metabolic diseases risks.
Citation: Andrea P, Maria D, Roda G, Roda E. Health coaching experience in Minerbio (Italy): Global impact on weight, BMI, waist circumference and blood pressure. Japanese J Gastroenterol Res. 2021; 1(8): 1037.
Introduction
Research has consistently shown that the Mediterranean diet is effective in reducing the risk of cardiovascular diseases and overall mortality [1,2]. Despite this evidence, Mediterranean diet underutilization is common. A study of nearly 26,000 women found that those who followed this Mediterranean diet had 25% less risk of developing cardiovascular disease over 12 years [3]. The study examined a range of underlying mechanisms that might account for this reduction, and found that changes in inflammation, blood glucose concentration, and body mass index were the biggest drivers. The PREDIMED study, a primary prevention trial including thousands of people with diabetes or other risk factors for heart disease, found that a Mediterranean diet supplemented with extra virgin olive oil or nuts and without any fat and calorie restrictions reduced the rates of death from stroke by around 30%. Risk of type 2 diabetes was also reduced in the PREDIMED trial [4].
Additionally, short-term results from a multi-component program indicate that the progressive epidemic of childhood obesity may be effectively modified by a school-based intensive intervention. Data from this study, proposed as a playful activity to children in a school district, indicate that the intervention was able to modify the time trend of progressive increase in BMI which is commonly observed in childhood [5].
Moreover, lifestyle changes aiming at healthy diet and routinary physical activity are needed for the prevention and treatment of type 2 diabetes, as well as in other metabolic disorders. Marchesini et al. followed 100 subjects with diabetes or obesity enrolled in a dance program and showed that dance may be an effective strategy to implement physical activity in motivated subjects with type 2 diabetes or obesity [6].
Several studies have demonstrated that a major portion of all chronic diseases could be prevented by diet, physical activity, and weight control. Health coaching has a pivotal role in primary care, helping patients to self-education. "Health coaching can be defined as helping patients gain the knowledge, skills, tools and confidence to become active participants in their care so that they can reach their self-identified health goals" [7]. A study from the University of Michigan enrolling 82 subjects, showed that a 12-week program consisting of telephone coaching with in-person visits at the beginning and end of the program targeting improvements in diet, physical activity, and/or sleep habits is a cost-effective method for improving the health of patient populations [8].
Rationale
We designed a year health coaching program which consists in dedicated physicians (called coaches) who strictly follow patients in their diet and lifestyle (physical exercises, alcohol and smoking behavior) over a one-year period. The overall goal of the program is to instruct patients' lifestyle to a Mediterranean diet and exercises to reduce cardiovascular disease risks, diabetes, and metabolic diseases' risks.
Material and methods
Study population
Patients' characteristics are summarized in (Table 1).
The sample consists of 62 subjects, 21 male (33.9%) and 41 female (66.1%), with an average age of 52 years (19–77); the average height of the patients was 169 centimeters (150–185). Mean weight was 75.4 Kg (43-112), with a BMI of 26.2 Kg/m2 (17.2-38.6), a waist circumference of 93.4 cm (61-130) and mean blood pressure values of 120/80 mmHg at the enrollment visit. Patients were classified in relation to BMI (Table 1). Twenty-seven patients had normal weight (45.8%), 18 were overweight (30.5%) and 13 obese (22%). Of the 13 obese patients, 5 were classified as class II obesity. In relation to the abdominal circumference guidelines, 45% of patients show high risk values (13 males and 15 females).
Patients were followed by a dedicated physician termed COACH. A pedometer was given to each patient and an application phone kit with instructions related to the Mediterranean diet and lifestyle such as alcohol and smoking consumption were also dedicated to each patient.
Patients received 2 outpatients assesment (time 0 and month 12) during the one-year study with arteriosus pressure, weight and waist circumference determination. During the first visit comorbidities and medications were also registered. Each week patients received one contact from the coach (by web or phone). Weight, exercises done during the week, pedometer evaluation, behavior were registered during these visits from the coach.
Table 1: Baseline characteristics of the study population (# 62).
| Sex | |
|---|---|
| Male | 21 (33.87%) |
| Female | 41 (66.13%) |
| Age (N.61), mean (range) | 48 (43–58.5) years |
| Height (N.59), mean (range) | 169 (150–185) cm |
| Weight (N.62), means (range) | 75.4 (43–112) kg |
| BMI (N.59), mean (range)* | 26.23 (17.22–38.57) Kg/m2 |
| underweight n (%) | 1 (1.7%) |
| normoweight, n (%) | 27 (45.8%) |
| overweight, n (%) | 18 (30.5%) |
| obese n (%) | 13 (22%) |
| class I | 8 (61.5%) |
| class II | 5 (38.5%) |
| Waist circumference (N.60), mean (range) | 93.4 (61-130) cm |
| male | 105 (91–130) cm |
| female | 86.7 (61–114) cm |
| Waist circumference and risk** | |
| male | |
| normal | 38.1% (95.4 cm) |
| high risk | 61.9% (111 cm) |
| female | |
| normal | 62.5% (78.1 cm) |
| high risk | 37.5% (101.1 cm) |
| Blood pressure | 120/80 mmHg |
| ≤120/80, n (%) | 34 (59.6%) |
| 120-130/80, n (%) | 15 (26.3%) |
| >130/80, n (%) | 8 (14%) |
* BMI: underweight if <18.5, normal weight if 18.5–24.9, overweight if 25–29.9, obesity if> 30 (class I obesity if 30–34.9, class II obesity> 35; ** the Guidelines define waist circumference values> 102 cm for males,> 88 cm for females at high risk.
Statistics
Samples followed a normal distribution. Categorical variables are reported as number (n) e percentage (%), while continuous variables such as mean and range (minimum value – maximum value). For the comparison between continuous variables the Paired t-test was used. The statistical analysis was conducted with StatView for Windows. Values of P < 0.05 were statistically significant.
Results
100% of the patients concluded the study. The characteristics of the entire population at the end of the program are summarized in Table 2. The average weight was 72.8 Kg (41–110), with a BMI of 25.2 Kg/m2 (16.4–37.8), the waist circumference was 89 (60–127), while the mean blood pressure values were 118/74 mmHg.
Patients were classified in relation to BMI (Table 2). 35 patients had normal weight at the end of the program (59.3%), 12 were overweight (20.3%) and 10 obese (16.9%) of which 3 within class II obesity.
27.9% of patients show high values risk according to the abdominal circumference guidelines (4 males and 13 females).
(Table 3) summarizes the global effects of the coaching program on the entire population: reduction in weight, BMI and waist circumference were statistically significant at the end of the course compared to initial values. Blood pressure is also reduced, especially diastolic.
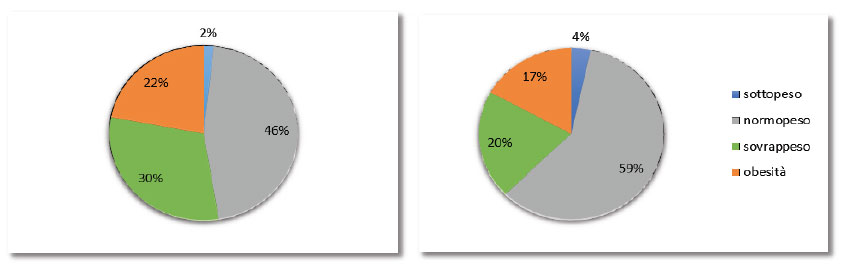
As shown in (Figure 1), there was an increase in normal weight patients (from 46% to 59%), with a reduction in overweight patients (from 30% to 20%) but above all with a reduction in the share of obese people (from 22% to 17%).
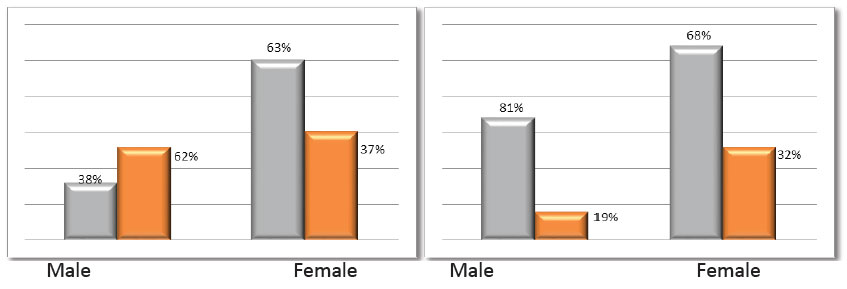
As shown in (Figure 2), there is a reduction in waist circumference, regarding "high risk" values, especially in the male population, from 62% at the beginning of the program to 19% at the end.
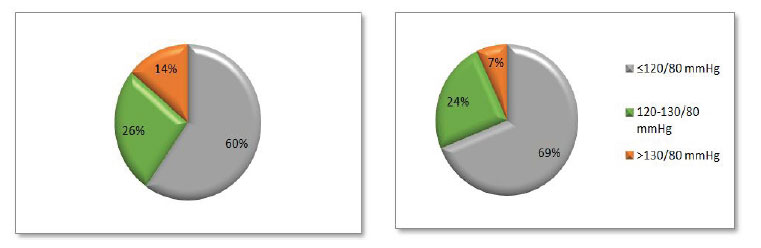
(Figure 3) shows an increase in patients with normal blood pressure (from 60% to 69%) with a significant reduction in patients with high blood pressure (from 14% to 7%).
Table 2: Characteristics of the study population at month 12 (# 62).
| Weight (N.62), mean (range) | 72.8 (41–110) kg |
| BMI (N.59), mean (range)* | 25.21 (16.42–37.83) Kg/m2 |
| underweight, n (%) | 2 (3.4%) |
| Normo weight, n (%) | 35 (59.3%) |
| overweight, n (%) | 12 (20.3%) |
| obese, n (%) | 10 (16.9%) |
| class I | 7 (70%) |
| Class II | 3 (30%) |
| Waist circumference (N.61), mean (range) | 89.0 (60-127) cm |
| Male (N.21), mean (range) | 100.4 (88–127) cm |
| Female (N.40), mean (range) | 83 (60–109) cm |
| Waist circumference and risk ** | |
| male (N.21) | |
| normal (N.17) | 81% (96.8 cm) |
| High risk (N.4) | 19% (115.5 cm) |
| Female (N.40) | |
| Normal (N.27) | 67.5% (76.2 cm) |
| High risk (N.13) | 32.5% (97.3 cm |
| Blood pressure | 118/74 mmHg |
| ≤120/80, n (%) | 40 (69.0%) |
| 120-130/80, n (%) | 14 (24.1%) |
| >130/80, n (%) | 4 (6.9%) |
* BMI: underweight if <18.5, normal weight if 18.5–24.9, overweight if 25–29.9, obesity if> 30 (class I obesity if 30–34.9, class II obesity> 35; ** the Guidelines define waist circumference values> 102 cm for males,> 88 cm for females at high risk.
Table 3: Coach program global modifications.
| Characteristic | Time 0 | 12 months | Variation | P |
|---|---|---|---|---|
| Wieight, kg, mean (range) | 75.4 (43–112) | 72.8 (41–110) kg | -3.3% | 0.0006 |
| BMI, Kg/m2, mean (range)* | 26.23 (17.22–38.57) | 25.21 (16.42–37.83) Kg/m2 | -3.4% | 0.0004 |
| Waist circumference, cm, mean (range) | 93.4 (61-130) | 89.0 (60-127) cm | -4.1% | <0.0001 |
| Arterious pressure | 120/80 mmHg | 118/74 mmHg | ||
| sistolic, mmHg, mean (range) | 120.1 (80–149) | 117.8 (80–143) | -1.5% | 0.056 |
| diastolic, mmHg, mean (range) | 76.10 (46–94) | 73.7 (48–96) | -2.4% | 0.019 |
Conclusion
100% of the patients concluded the study. In this pilot study, 80% of the patients registered a significant (p<0.05) reduction of the weight, 78% increased physical activity and 90% reported a better behavior measured with quality-of-life scores. Half of the patients stopped smoking and alcohol consumption and the remaining decreased number of daily cigarettes and alcohol consumption.
30% of the subject enrolled in the program were older than 70 years and didn't experience any femoral fracture over the one-year program.
Overall, all the patients experienced a significant decrease of the waist circumference and a trend to a reduction in the blood pressure which have been shown to correlate with decrease in cardiovascular and metabolic risk.
This preliminary study shows that a dedicated health program with specialized physician (coach) who follow strictly patients' diet and physical activity is a tool of primary prevention with low costs and high effectiveness over the time.
References
- Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009 Mar 3; 119(8):1093-100.
- Lopez-Garcia E, Rodriguez-Artalejo F, Li TY, Fung TT, Li S, Willett WC, Rimm EB, Hu FB. The Mediterranean-style dietary pattern and mortality among men and women with cardiovascular disease. AJCN. 2013 Oct 30; 99(1):172-80.
- Ahmad S, Moorthy MV, Demler OV, Hu FB, Ridker PM, Chasman DI, Mora S. Assessment of Risk Factors and Biomarkers Associated With Risk of Cardiovascular Disease Among Women Consuming a Mediterranean Diet. JAMA Network Open. 2018 Dec 7; 1(8):e185708.
- Estruch R, Ros E. The role of the Mediterranean diet on weight loss and obesity-related diseases. Rev Endocr Metab Disord. 2020 Sep; 21(3):315-327.
- Centis E, Marzocchi R, Di Luzio R, Moscatiello S, Salardi S, Villanova N, Marchesini G; G. C. Croce School of Health Promotion. A controlled, class-based multicomponent intervention to promote healthy lifestyle and to reduce the burden of childhood obesity. Pediatr Obes. 2012 Dec; 7(6):436-45.
- Mangeri F, Montesi L, Forlani G, Dalle Grave R, Marchesini G. A standard ballroom and Latin dance program to improve fitness and adherence to physical activity in individuals with type 2 diabetes and in obesity. Diabetol Metab Syndr. 2014 Jun 22; 6:74.
- Bennett HD, Coleman EA, Parry C, Bodenheimer T, Chen EH. Health coaching for patients with chronic illness. Fam Pract Manag. 2010 Sep-Oct; 17(5):24-9.
- Djuric Z, Segar M, Orizondo C, Mann J, Faison M, Peddireddy N, Paletta M, Locke A. Delivery of Health Coaching by Medical Assistants in Primary Care. J Am Board Fam Med. 2017 May-Jun; 30(3):362-370.