Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 1
Jejunal diverticular disease complicated with spontaneous perforation: A rare case of acute abdomen and literature review
Flávio Silano*; Vanessa Costa Neves; Ricardo Bandeira de Melo Amaral; Rodolfo Carvalho Santana; Paulo Cezar Galvão do Amaral
Department of Surgery of the Upper Digestive System, Hospital da Cidade Group, Salvador, Bahia, Brazil.
*Corresponding Author: Flavio Silano
Department of Surgery of the Upper Digestive System, Hospital da Cidade Group, Salvador, Bahia, Brazil.
Email: sdesilano@gmail.com
Received : Sep 18, 2021
Accepted : Nov 15, 2021
Published : Nov 18, 2021
Archived : www.jjgastro.com
Copyright : © Silano F (2021).
Abstract
Introduction: The jejunal diverticular disease is an uncommon clinical pathology. In general, these diverticula are an incidentaloma found on imaging exams that can be seen in elective surgeries for other purposes. In a minority of cases it causes symptoms which result from serious complications such as perforation.
Case report: A 56-year-old male patient, previously healthy and without comorbidities, was admitted to the emergency department due to abdominal pain which had started 24 hours ago, without improvement. On examination, the patient was in pain and in Mohammedan prayer's position in bed and had a distended abdomen with signs of peritoneal irritation. An abdominal tomography showed massive distension of intestinal loops and free fluid in the peritoneal cavity. He underwent exploratory laparotomy which showed multiple diverticula in the jejunum and one of them was perforated. Segmental enterectomy with primary anastomosis was performed.
Conclusion: Complicated jejunal diverticular disease should be ranked among the differential diagnoses in acute perforating abdomen. Segmental jejunal resection is the treatment of choice.
Keywords: small bowel diverticulum; jejuno-ileal diverticula; diverticulitis; perforation; acute abdomen; surgery.
Citation: Silano F, Neves VC, Amaral RBM, Santana RC, Amaral PCG. Jejunal diverticular disease complicated with spontaneous perforation: A rare case of acute abdomen and literature review. Japanese J Gastroenterol Res. 2021; 1(8): 1036.
Introduction
Jejunal diverticular disease (JDD) is rare and found in 0.3 to 4.5% of intestinal diverticula [1]. Its incidence is higher in males, with a prevalence in those who are over 60 years old [2,3]. Most patients are asymptomatic and the rule for diagnosis has been incidentalomas found on imaging exams, in explorations of the abdominal cavity which are performed for elective or urgent surgeries and in autopsies [2,4]. However, in around 10% of cases, patients may present some type of complication such as: abdominal pain resulting from an inflammatory process, bleeding, obstruction and perforation with risk of death [2]. The authors present here a case report of surgical resection of the jejunal segment for diverticular disease, complicated by perforation, in an adult male patient, conducted in a single center with experience in digestive surgery.
Case report
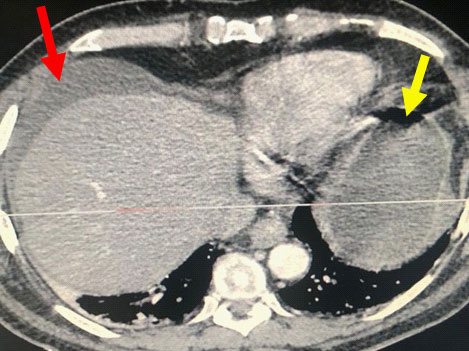
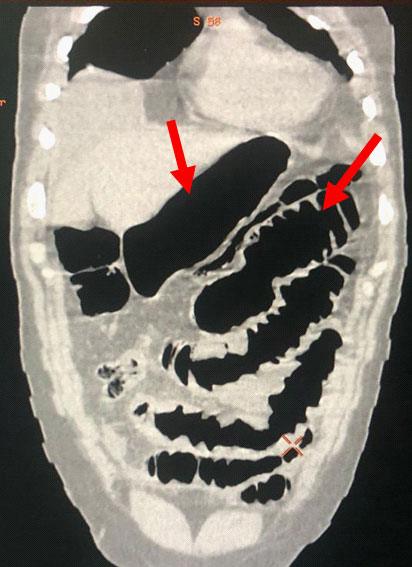
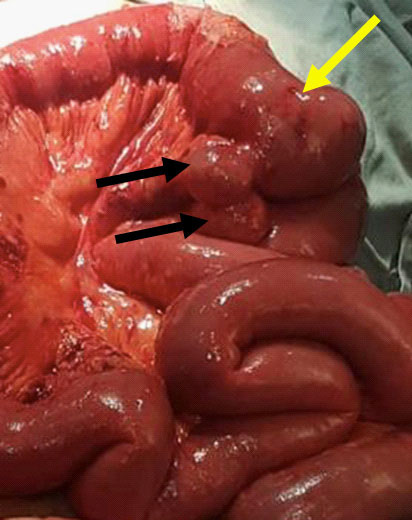
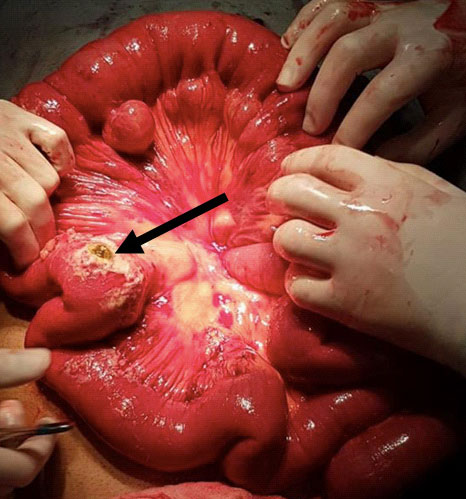
A 56-year-old male patient, who was previously healthy, was admitted to the emergency room of Hospital da Cidade – Salvador – Bahia – Brazil due to diffuse abdominal pain that started 24 hours before admission, with progressive worsening and intensity 9, on a 0-10 scale. During physical examination he was tachycardic (HR > 90 bpm), tachypneic (RR > 20), normotensive, in antalgic position and had distended abdomen with diffuse pain on decompression and poor response to opioid analgesics. He did not have systemic inflammatory response syndrome (SIRS) and laboratory tests, including white blood cell count and pancreatic enzymes were normal. The radiological routine for acute abdomen was not clarifying and thus, contrasted Computed Tomography (CT) of the abdomen was performed, showing: Free fluid in the abdominal cavity and important jejunal and gastric distension (Figures 1 & 2). The distension of the small intestine made it impossible to access the abdominal cavity by laparoscopy. Exploratory Laparotomy (EL) was performed which showed large amounts of enteric fluid in all abdominal quadrants, significant edema of the small bowel loops and multiple jejunal diverticula (Figure 3). One of them was perforated and located 30 cm from the Treitz angle (Figure 4), which was defined by segmental enterectomy of approximately 20cm (figure 5). Primary lateral-lateral anastomosis was performed using a linear stapler for intestinal reconstruction and cleaning of the abdominal cavity until clear return of the aspirate. There was a postoperative period in the intensive care unit (ICU) for 3 days, due SIRS and necessity of the clinical and laboratorial surveillance. During that time, nutritional therapy with Total Parenteral Nutrition (TPN) was started early. After improvement in abdominal distension and removal of the nasogastric tube on the 7th day after surgery (POD), an oral liquid diet without residues was introduced. There were no postoperative complications or need for surgical re-approach. Finally, the patient was discharged on the 11th POD with a mild oral diet, without complaints and with a normal bowel rhythm. There was no readmission.
Discussion
The jejunal diverticular disease is an uncommon pathology, with an annual incidence ranging from 0.3% to 2.3% [5]. The first reports are from 1794, by Sommerling [1] and some authors quote autopsy findings ranging from 0.2 to 1.3% [4]. The etiology is poorly understood and theoretically there is an abnormality in the neuromotor innervation causing intestinal dyskinesia. However, it is uncertain [6]. With an abnormal increase in intraluminal pressure in weak points of the small intestine, false diverticula are formed with pulsation due to the penetration of blood vessels in the wall [7].
Symptoms
Many people with jejunal diverticular disease do not know they have it because they are asymptomatic or have nonspecific symptoms such as: dyspepsia, diarrhea, occasional nausea and vomiting, among others [2,8]. In 10% of cases, the symptoms can be relevant, causing digestive hemorrhage, acute perforating abdomen, sepsis and even death [2,9].
Acute and chronic complications of diverticular disease of the jejunum
Inflammation and perforation are the most common acute complications of this disease [10]. The pathophysiology of the inflammatory event may be limited and without clinical repercussions, but there is a risk of evolution to ulcer, necrosis and perforation of the diverticulum in 2.3% to 6.4% of cases, with serious consequences [13,14]. Anatomically, the fundus of the jejunal diverticulum is close to branches of the mesenteric vessels and this can lead to acute and chronic hemorrhagic complications. However, it is much less frequent than inflammation / diverticular perforation [10]. Other complications reported in the literature are: Intestinal obstruction caused by a voluminous diverticulum with liquid content in its interior causing extrinsic compression of the intestinal loop, acute volvulus or even intestinal intussusception and malabsorption of vitamin B12 caused by stasis in the diverticular lumen and bacterial overgrowth which can generate megaloblastic anemia in the long term [10]. In our case report, the patient was admitted due to sudden, severe abdominal pain, which did not improve with analgesics at home, and when he arrived at the hospital, he had a tense, distended abdomen, with signs of peritoneal irritation and was in Mohammedan prayer's position in bed. Classic signs of a perforating acute abdomen.
Diagnosis
In our opinion, it is uncommon to suspect diverticular disease of the jejunum in oligosymptomatic patients with dyspeptic complaints and even in complications. Perforation, acute and/or chronic bleeding is not usually part of the differential diagnoses. Exception is found in radiological history that already highlighted DJD as a previous incidentaloma. In this case report, the patient had a clinical picture of a perforating acute abdomen and our main suspicion was a perforated peptic ulcer disease. The surgical approach would not be changed, but the patient and family would get clear explanation about the possibility of resection of the intestinal loop segment, anastomosis and risk of dehiscence.
Treatment
For asymptomatic patients with jejunal diverticular disease, the literature recommends parsimony in conduction, avoiding initial resections, which can often be extensive in cases of multiple diverticula [10-12]. We corroborate this fact, since the highest incidence of this pathology is in the elderly. Performing resections in asymptomatic patients as a preventive manner can cause unnecessary surgical morbidity if we consider that the minority will present complications due to the natural history of the jejunal diverticular disease. For cases with some type of complication, such as our patient, who had a perforating acute abdomen, surgical treatment is mandatory and should not be postponed.
Conclusion
Complicated jejunal diverticular disease should be part of the differential diagnoses in patients with acute abdomen in emergency, especially when there is suspicion of perforation in hollow viscera. In those cases with free cavity perforation, segmental surgical resection and primary anastomosis seem to be a safe strategy.
References
- Sehgal R, Cheung CX, Hills T et al: Perforated jejunal diverticulum: A rare case of acute abdomen. J Surg Case Rep, 2016; 10:1–3.
- El-Haddawi F, Civil ID: Acquired jejuno-ileal diverticular disease: a diagnostic and management challenge. ANZ J Surg, 2003; 73:584–89.
- Liu CY, Chang WH, Lin SC et al: Analysis of clinical manifestations of symptomatic acquired jejunoileal disease. World J Gastroenterol, 2005; 11(35):5557–60.
- Noer T: Non-Meckelian diverticula of the small bowel: The incidence in an autopsy material. Acta Chir Scand, 1960; 120:175–79.
- Lebert P, Millet I, Ernst O, Boulay-Coletta I, Corno L, Taourel P, et al. Acute jejunoileal diverticulitis: multicenter descriptive study of 33 patients. AJR Am J Roentgenol. 2018; 210(6):1245–51
- Kongara KR, Soffer EE. Intestinal motility in small bowel diverticulosis: a case report and review of the literature. J Clin Gastroenterol. 2000; 30(1):84–6.
- Natasha Leigh, Brianne J. Sullivan, Roi Anteby, Susan Talbert. Perforated jejunal diverticulitis: a rare but important differential in the acute abdômen. Surgical Case Reports (2020); 6:162
- Kassir R, Boueil-Bourlier A, Baccot S et al: Jejuno-ileal diverticulitis: Etiopathogenicity, diagnosis and management. Int J Surg Case Rep, 2015; 10:151–53.
- Bruno Augusto Alves Martins, Rosana Rodrigues Galletti, Júlio Marinho dos Santos Neto, Caroline Neiva Mende. A case of perfurative diverticulum: An Unexpected Cause of Pneumoperitoneum in a Patient with an Acute Abdomen. Am J Case Rep, 2018;19:549-55
- Falah El – Haddawi and Ian D. Civil. Acquired Jejuno-ileal Diverticular disease: A diagnostic and management challenge. ANZ J. Surg. 2003; 73:584–589.
- Altemeier WA, Bryant LR, Wulsin JH. The surgical significance of jejunal diverticulosis.Arch. Surg.1963; 86:732–44.
- Akhrass R, Yaffe M, Fischer C, Ponsky J, Shuck JM. Smallbowel diverticulosis: Perceptions and reality. J. Am. Coll. Surg.1997; 184: 383–8.
- Herrington JL. Perforation of acquired diverticula of the jejunum and ileum. Surgery 1962; 51:426–34.
- Alice Maria Ramistella, Massimo Brenna, Fabrizio Fasolini, Marco de Monti. Jejuno-ileal diverticulitis: A disorder not to underestimate. International Journal of Surgery Case Reports 58 (2019); 81–84.