Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 1
Giant gastric trichobezoar: Case report
N Daniel Velasco Hernández*; Héctor R Horiuchi; Santiago B De Battista; Lucas A Rivaletto; Matías Sabbatini
Departament of Surgery, University Hospital General San Martín of La Plata, Buenos Aires, Argentina.
*Corresponding Author: N Daniel Velasco Hernández
Departament of Surgery, University Hospital General San Martín of La Plata, Buenos Aires, Argentina.
Email: ndvelascohernandez@gmail.com &
daniels84@hotmail.com
Received : Sep 04, 2021
Accepted : Oct 08, 2021
Published : Oct 15, 2021
Archived : www.jjgastro.com
Copyright : © Hernández NDV (2021).
Introduction
A trichobezoar is a rarely encountered mass of hair, wool, and similar material in the stomach and intestine of some patients with trichotillomania and trichophagia. The accumulated hair within the stomach and intestine is resistant to digestion, which occasionally presents as trichobezoar-induced bowel or gastric outlet obstruction. Trichobezoars are more common in paediatric age than adults, with up to 90% occurring in girls [1-3]. This report aims to describe the case of a young woman with an obstructive trichobezoar of the stomach and duodenum.
Citation:Hernández NDV, Horiuchi HR, Battista SBD, Rivaletto LA, Sabbatini M. Giant gastric trichobezoar: Case report.Japanese J Gastroenterol Res. 2021; 1(6): 1026.
Case presentation
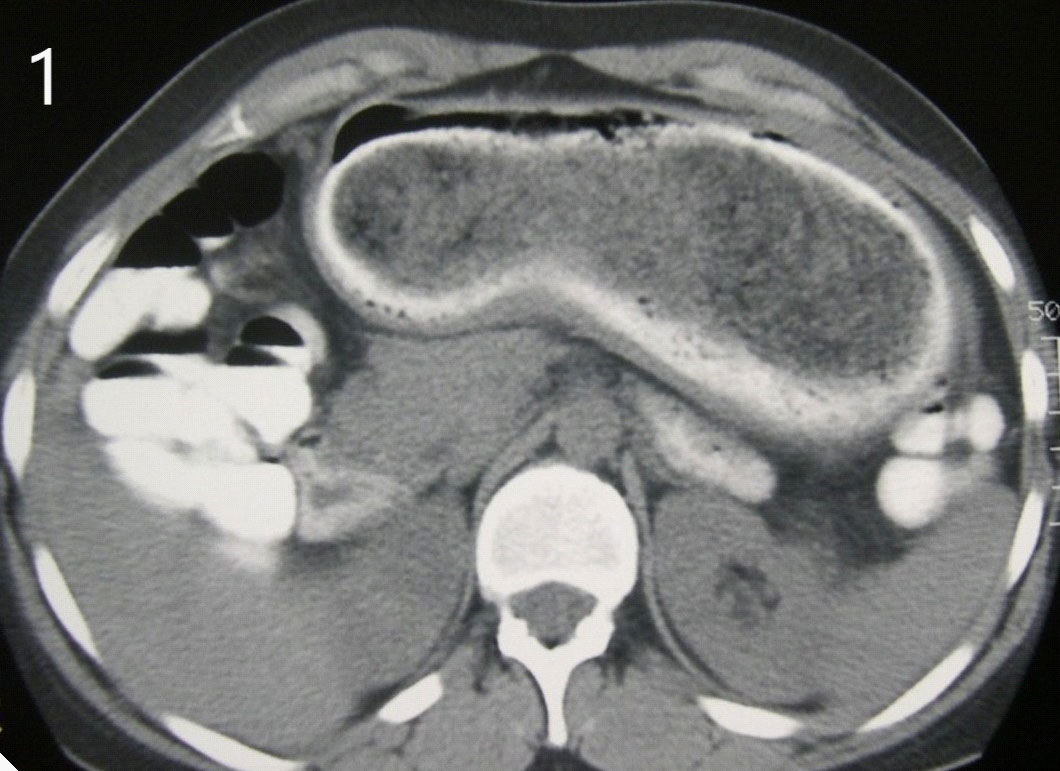
A 27-year-old woman presented to the emergency room with epigastric abdominal pain and intermittent vomiting of 4 days of evolution. The patient has a history of anxiety symptoms. Dehydration and a palpable hard-elastic mass in the epigastric region were observed during the physical examination. The laboratory analysis did not show significant alterations. In imaging studies, occupied gastric dilation with a heterogeneous formation was evidenced inside. Hospitalization (Figure 1) was decided, and an upper digestive video endoscopy was performed, through which an abundance of hairs was observed inside the stomach without the possibility of progression to the body and gastric antrum. Open surgery was decided, a median supraumbilical laparotomy was performed, a gastrostomy and a giant trichobezoar were extracted (Figures 2 & 3). The patient progressed favourably; She began with fluid intake at 24 hours and was discharged without complications at 72 hours. The patient was referred to control by surgery, gastroenterology and mental health departments.
Discussion
The trichobezoar represents 55% of all bezoars, more frequent in women under 30 years of age, as in the case presented. Trichophagia is the unfailing antecedent of a trichobezoar; it is a prevention of appetite related to pica, and that can be determined by psychic alterations, among them, oligophrenia, psychosis, neurosis, autism or psychomotor retardation. Hair can be obtained from siblings, pets, dolls, brushes, or the patients themselves [4,5]. The scalp is the most affected, in the form of segmental alopecia due to hair traction, but the origin may be the eyebrows and eyelashes. Initially, abdominal pain usually occurs in the epigastrium and in the left upper quadrant, followed by anorexia, weight loss, halitosis, vomiting, and diarrhea. In addition, when they are large, they usually manifest as an abdominal mass in the epigastric region, such as the patient we have presented [6-8]. Complications may be due to obstruction either at the level of the pylorus, duodenum or jejunum. However, they can also be traumatic, manifesting with ulcers, bleeding and perforation [9,10].
In most cases, they are unique, and only 15% spread to the small intestine. The diagnosis is difficult because the patient usually denies or hides trichophagia or trichotillomania, which makes clinical suspicion difficult; Diagnostic methods include ultrasonography, contrast-enhanced CT, and gastrointestinal endoscopy. Abdominal ultrasonography can show an intragastric mass of high-amplitude echoes, with posterior acoustic shadowing, and barium-contrasted radiography shows us a typical "honeycomb" image, caused by part of the barium that is retained in the bezoar; however, CT is one of the more specific methods, showing a heterogeneous image that dilates the gastric cavity. Upper endoscopy is the test of choice, allowing us to observe the trichobezoar lodged in the gastric cavity directly and thus determine the therapeutic procedure [11,12].
Conclusion
In conclusion, the trichobezoar, once diagnosed, requires an immediate approach for its removal. This can be able for endoscopic, by fragmentation, or laparoscopic if it is small or by laparotomy in large ones. In turn, once the acute picture has been overcome, these types of patients must be approached thoroughly by surgeons, gastroenterologists, and a mental health team.
References
- Zhi-Hui Dong, Feng Yin, Shi-Lin Du, Zhe-Heng Mo. Giant gastroduodenal trichobezoar: A case report. World J Clin Cases 2019; 7: 3649-3654.
- Hidayatullah Hamidi, Marzia Muhammadi, Bismillah Saberi, Mohammad Arif Sarwari. A rare clinic entity. Huge tricobezoar. International Journal of Surgery Case Reports. 2016; 28: 127–130.
- Ibrahim Yetim, Orhan Veli Ozkan, Ersan Semerci and Recep Abanoz. Unusual cause of gastric outlet obstruction: giant gastric trichobezoar: a case report. Cases Journal. 2008; 1: 399.
- A.A. Ibuowo, A. Saad, T. Okonkwo, Giant gastric trichobezoar in a young female, Int. J. Surg. 2008; 6: e4–e6.
- Fallon SC, Slater BJ, Larimer EL, Brandt ML, Lopez ME. The surgical management of Rapunzel syndrome: a case series and literature review. J Pediatr Surg. 2013; 48: 830-834.
- Meriam Sabbah, Asma Ouakaa, Norsaf Bibani, Dorra Trad, Dalila Gargouri. Gastric trichobezoar revealed by epigastric mass. Presse Med. 2019; 48: 588-589.
- Coulter R, Antony MT, Bhuta P, Memon MA. Large gastric trichobezoar in a normal healthy woman: case report and review of pertinent literatura. South Med J. 2005; 98: 1042-4.
- Rachel M Zent , C Clay Cothren, Ernest E Moore. Gastric trichobezoar and Rapunzel síndrome. J Am Coll Surg. 2004; 199: 990.
- AR. Jensen, CT Trankiem, S. Lebovitch, H. Grewal, Gastric outletobstruction secondary to a large trichobezoar, J. Pediatr. Surg. 2005; 40: 1364–1365.
- Jones GC, Coutinho K, Anjaria D, Hussain N, Dholakia R. Treatment of recurrent Rapunzel síndrome and trichotillomania: case report and literature review. Psychosomatics. 2010; 51: 443-446.
- Morales-Fuentes B, Camacho-Maya U, Coll-Clemente FL, Vázquez-Minero JC. Trichotillomania, recurrent trichobezoar and Rapunzel syndrome: case report and literature review. Cir. 2010; 78: 265-266.
- Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV. Trichobezoars in the stomach and ileum and their laparoscopy-assisted removal: A bizarre case. Singapore Med J. 2007; 48: e37-e39.