Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 1
Invasive candida infection after bariatric surgery for morbid obesity presenting as late anastamotic leak
Jayanth Moode; KASSN Kalyan*; Lakshmi Kona
Department of GI and Minimal Access Surgery, Gleneagles Global Hospital, Hyderabad.
*Corresponding Author: KASSN Kalyan
Department of GI and Minimal Access Surgery, Gleneagles Global Hospital, Hyderabad.
Email: adityakalya@gmail.com
Received : Sep 10, 2021
Accepted : Oct 07, 2021
Published : Oct 14, 2021
Archived : www.jjgastro.com
Copyright : © Kalyan KASN (2021).
Abstract
Introduction: Gastrointestinal (GI) leaks are one of the most dreaded complications following bariatric surgery because of the difficulty in diagnosing them and the associated increased morbidity and mortality.
Case report: Presenting one such case of 49 yr old gentleman who was on follow-up post bariatric surgery presented lately as acute abdomen and diagnosed as GI perforation and further evaluation and procedure carried out.
Discussion: GI leakage after bariatric surgery has been identified as an independent risk factor associated with perioperative death. This highlights the importance of high index of suspicion for diagnosis of this potentially lethal complication. A positive radiology should not be awaited for before exploring patients in whom the diagnosis is still unclear.
Conclusion: Histopathologic examination (HPE) remains one of the major diagnostic tools in mycology because it permits rapid, presumptive identification of fungal infections, even when blood cultures are negative. There are different ways to manage leaks, depending on the magnitude of the collection and the clinical presentation.
Keywords: surgical pathology; gastrointestinal candidiasis; diagnosis; mini gastric bypass; bariatric surgery; candida.
Citation:Moode J, Kalyan KASSN, Kona L. Invasive candida infection after bariatric surgery for morbid obesity presenting as late anastamotic leak. Japanese J Gastroenterol Res. 2021; 1(5): 1025.
Introduction
Gastrointestinal (GI) leaks are one among the most feared complications following bariatric surgery due to the problem in diagnosing them and therefore the associated increased morbidity and mortality. Difficulty in diagnosis is said to be due to the nonspecific systemic symptoms and limitations in most radiological studies. Treatment modalities range from observation to reoperation. GI leak after bariatric surgery is not an uncommon complication and one that can be expected to occur at some point in every bariatric surgeon's experience.
Underlying comorbidities, such as immunosuppression, cancer, the frequently malnourished state of critical care patients, administration of total parenteral nutrition, and use of intravenous catheters, are additional factors that tend to increase the frequency of Candida colonization in bariatric surgery [1,2]. The broad goal of treatment continues to be administration of safe and efficacious antifungal therapy as soon as possible. The developments and ongoing studies of dosing, toxicity and resistance development may play a role in future changes to the treatment of invasive candidiasis [3].
Case report
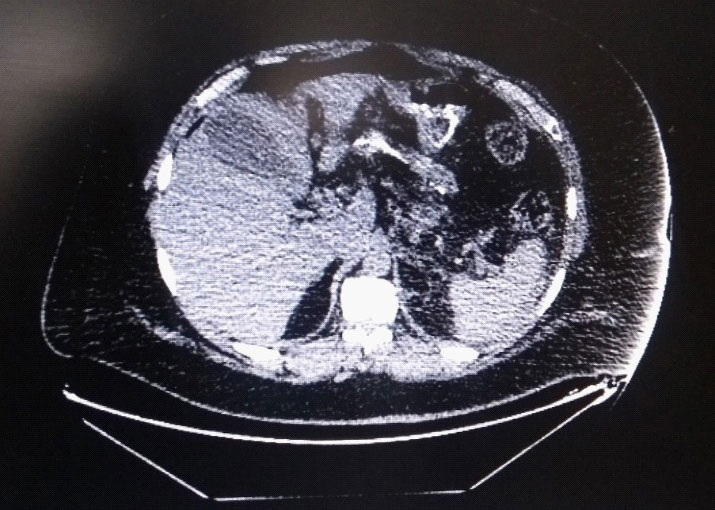
49 yr old gentleman, who underwent Mini gastric bypass for morbid obesity in 2013, presented with chief complaints of pain abdomen since 3 days, more in the epigastrium, radiating to back, associated with breathlessness and left sided chest pain. His BMI was 44.5. The patient was vitally stable and afebrile. His abdomen was soft, non-distended, diffuse tenderness was present and there was no organomegaly. Computed Tomography (CT) abdomen revealed pneumoperitoneum with small volume collection in perisplenic region. Efferent jejunal loop appeared mildly edematous with few inter bowel foci of trapped air (Figure 1). Hence patient was taken up for diagnostic laparoscopy.
Intra operative findings
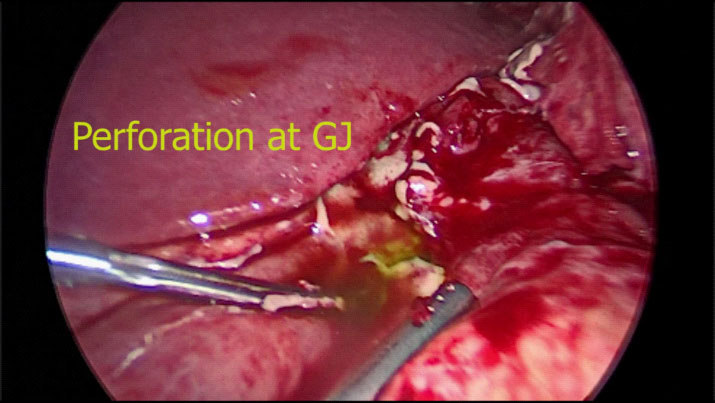
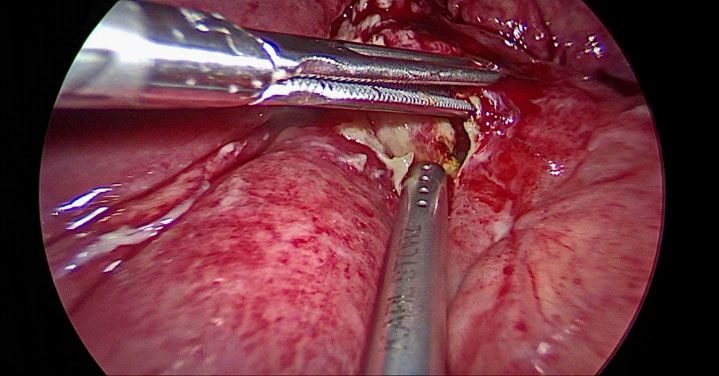
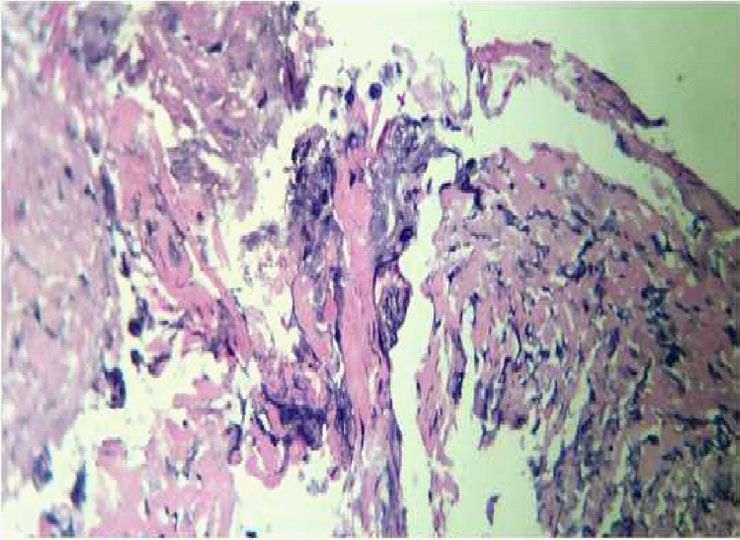
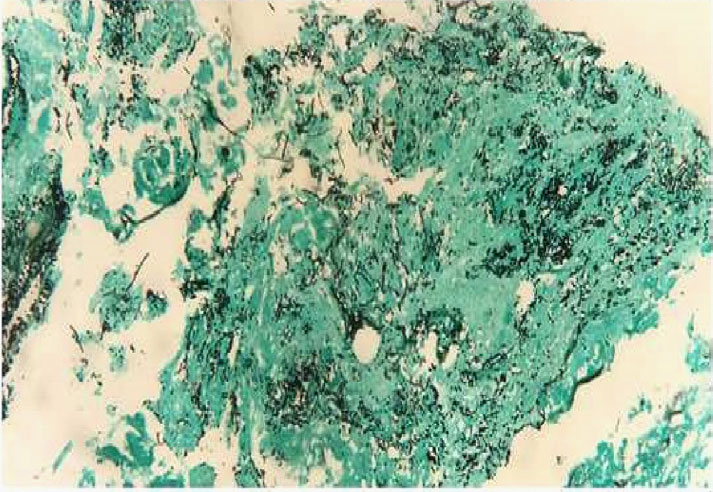
There was a 1 X 1 cm perforation at the gastrojejunostomy (GJ) anastomotic site (Figure 2 and 3). Multiple omento-enteric adhesions were present. Methylene blue test revealed a leak present at the GJ site. Primary closure of defect done after freshening of the edges and an omental patch repair was done. Ulcer edges were sent for histopathological examination (HPE) which showed infectious etiology with candida & actinomyces seen (Figure 4 and 5). Patient was given fluconazole 400 mg intravenously twice daily initially and later switched on to oral tablets for 2 weeks.
Discussion
Candida albicans is the most common cause of fungal sepsis, representing 35% to 60% of isolates. GI leakage after bariatric surgery has been identified as an independent risk factor associated with perioperative death [4]. Gastrographin upper GI series examinations are helpful to determine leaks at the gastro-jejunostomy or upper gastric pouch staple line. However, they cannot definitively rule out leaks in other locations. Although abdominal CT scan was positive in this case important limitations exist in its use and accuracy [5,6]. A positive imaging finding should not be awaited before exploring patients in whom the diagnosis is still unclear. In many studies, percutaneous drainage was very helpful in the control of leaks after bariatric surgery [7]. Isolated candida species exhibit varying levels of susceptibility to antifungal drugs. Histopathologic examination remains one of the major diagnostic tools because it permitsrapid, presumptive identification of fungal infections [8].
Conclusion
Histopathologic examination remains one among the main diagnostic tools in mycology because it permits rapid, presumptive identification of fungal infections, even when blood cultures are negative. There are several methods of managing anastamotic leaks, depending on the magnitude of the collection and the clinical presentation. Patients who present early with tachycardia and unilateral decrease in breath sounds warrant an exploratory laparoscopy inspite of a negative contrast test.
Declaration
Conflict of interest: The authors declare no conflict of interest.
Authors' contributions: All authors contributed equally to the paper.
References
- Edwards JE, Jr, Bodey GP., Bowden RA, et al. International conference for the development of a consensus on the management and prevention of severe candidal infections. Clinical Infectious Diseases. 1997; 25: 43–62.
- Blot SI, Vandewoude KH, De Waele JJ. Candida peritonitis. Current Opinion in Critical Care. 2007; 13: 195–199.
- Matteo Bassetti, Elda Righi, Philippe Montravers, Oliver A Cornely .Journal of Antimicrobial Chemotherapy. 2018; 73: i14–i25.
- AZ. Fernandez Jr, E.J. DeMaria, D.S. Tichansky, J.M. Kellum, L.G. Wolfe, J.Meador, et al.Multivariate analysis of risk factors for death following gastric bypass for treatment of morbid obesityAnn Surg. 2004; 239: 698-703.
- R. Gonzalez, MG. Sarr, CD. Smith M. Baghai, M. Kendrick, S. Szomstein, et al. Diagnosis and contemporary management of anastomotic leaks after gastric bypass for obesity. J Am Coll Surg. 2007; 204: 47-55.
- EH. Livingston Complications of bariatric surgery Surg Clin N Am. 2005; 85: 853-868.
- Csendes, P. Burdiles, A.M. Burgos, F. Maluenda JC. Diaz Conservative management of anastomotic leaks after 557 open gastric bypasses .Obes Surg. 2005; 15: 1252-125.
- Ohrmalm C, Eriksson R, Jobs M, Simonson M, Strømme M, et al. Variation-tolerant capture and multiplex detection of nucleic acids: application to detection of microbes. J Clin Microbiol. 2012; 8: 3208–3215.