Japanese Journal of Gastroenterology Research
Case Report - Open Access, Volume 1
Large primary retroperitoneal mucinous cystadenoma managed laparoscopically: Case report and literature review
Salah Termos1,*; Fahad AlGhareeb1; Mohamad AlHunaidi1; Fahad AlAbdulghani2; Ahmad AlJafar1; Ali AlQattan1; Ahmad Essam AlMulla1; Ayman Adi3; and Afaq Mahmoud AlKhalil1
1Department of Surgery, Al-Amiri Hospital, Kuwait.
2Department of Radiology, Al-Amiri Hospital, Kuwait.
3Department of Pathology, Al-Amiri Hospital, Kuwait.
*Corresponding Author: Salah Termos
General & HPB surgeon Al-Amiri Hospital, Kuwait, 25 Arabian Gulf Street, Kuwait City, 13041.
Tel: +96567782204
Fax: +96522464727
Email: salahtermos@gmail.com
Received : Aug 29, 2021
Accepted : Sep 20, 2021
Published : Sep 22, 2021
Archived : www.jjgastro.com
Copyright : © Termos S (2021).
Abstract
Background: Retroperitoneal cystic lesions (RCLs) are uncommon clinical findings that arise within the retroperitoneal compartments and account for various etiologies. They can be benign or malignant in nature and may present with different manifestations.
Case report: A 55-year-old woman presented with nonspecific right sided abdominal pain. Ultrasound detected a large cyst in the right retroperitoneal region, computed tomography revealed a large well-defined cystic lesion measuring 13 X 9 X 6 cm in the right posterior peritoneum extending from the subhepatic area to the right pelvis. Laparoscopic complete resection performed with uneventful perioperative course. Histopathologic findings were suggestive of mucinous cystadenoma.
Conclusion: Primary Retroperitoneal Mucinous Cystadenoma (PRMC) is an extremely rare pathology that can pose some challenge for clinicians. Awareness of this entity can help us in establishing the diagnosis and provide an optimal management. Although laparotomy is considered the standard approach of huge mucinous cystadenomas; laparoscopic surgery can be a safe and adequate therapeutic option.
Keywords: retroperitoneal cystic lesions (RCL); primary retroperitoneal mucinous cystadenomas (PRMCs); cystadenoma; mucinous; laparoscopy.
Citation:Termos S, AlGhareeb F, AlHunaidi M, AlAbdulghani F, Jafar A, et al. Large primary retroperitoneal mucinous cystadenoma managed laparoscopically: Case report and literature review. Japanese J Gastroenterol Res. 2021; 1(5): 1021.
Introduction
Retroperitoneal Cystic Lesions (RCLs) are uncommon masses that arise within the retroperitoneal space but outside the organs within that compartment. The differential diagnosis is wide and it can be cystic or solid, benign or malignant [1].
Mucinous cystadenomas account for 1% of benign epithelial neoplasms; however Primary Retroperitoneal Mucinous Cystadenomas (PRMCs) are extremely rare clinical finding, less than 50 cases have been reported and majority of them weremanaged by laparotomy. An accurate preoperative diagnosis is difficult to establish and the surgical option depends upon the degree of suspicion of malignancy and expertise [2].
We describe the case report of a large primary retroperitoneal mucinous cystadenoma that was successfully managed by laparoscopic resection.
Case presentation
We report the case of a 55-year-old woman, known to have hypothyroidism presented for a mild dull aching right sided abdominal pain radiating to the back. Patient reported no gastrointestinal or urinary symptoms and denied any fever or weight loss. She had no previous surgery and her gynecologic history was unremarkable.
Physical examination revealed normal vital signs. System review elicited no jaundice, edema, or lymphadenopathy but only a mild right-sided abdominal fullness; otherwise soft and lax with no tenderness. Routine laboratory investigation (complete blood count, renal function, liver function) were in normal ranges. Tumor markers (CEA, CA 19.9, CA 125, AFP) were all within normal values. Hydatid serology was negative.
Ultrasound showed small gallbladder polyps and a large cystic lesion in the right abdominal cavity. Contrast enhanced Computed Tomography (CT scan) scan demonstrated a 13 X 9 X 6 cm well-defined fluid filling cystic lesion with fine wall calcifications located in the right retroperitoneal compartment. This lesion is abutting the lower surface of the right kidney, seen extending from inferior border of the right liver lobe to the right psoas muscle. No infiltration to the adjacent organs and no direct attachment to the right ovary noted (Figure 1).
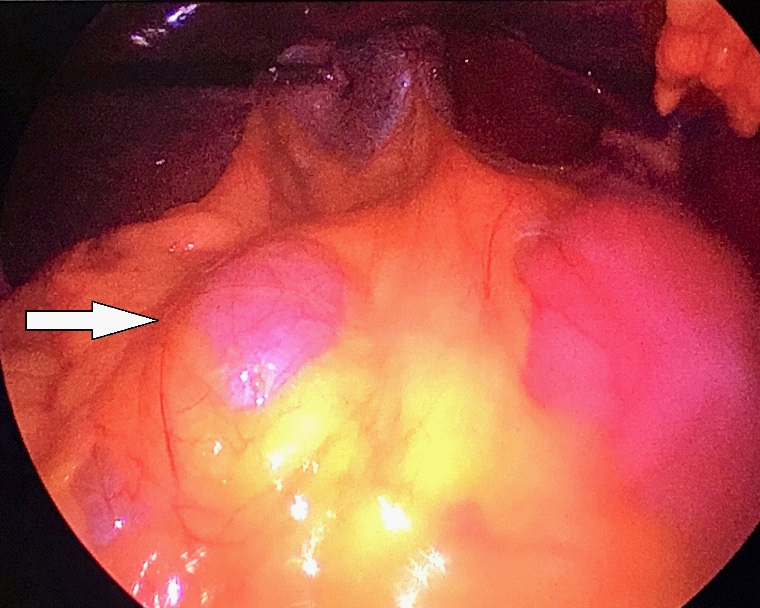
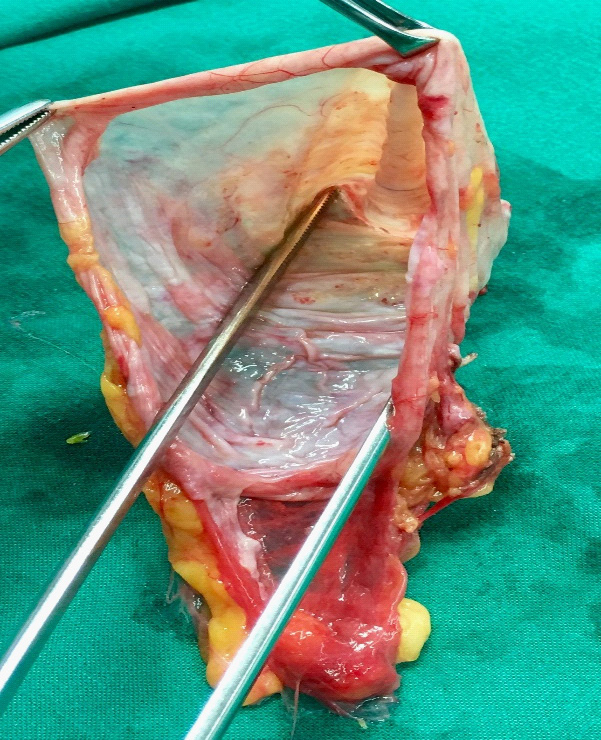
Multidisciplinary team (MDT) meeting recommended to attempt laparoscopic approach; since investigations revealed no biologic or radiologic potentially malignant features. Patient was consented for laparoscopic cholecystectomy and resection of the cystic mass with the possibility of conversion to laparotomy. She was placed in the reverse Trendelenburg with right up tilt position and the procedure was performed using three trocars only (two 5 mm and one 10 mm ports). Initial exploration revealed a large bulge within the mesentery of the right colon (Figure 2). Liver and peritoneal surfaces were examined and noted no abnormality. Adequate exposure was attained using Cattel maneuver (medial visceral rotation of right-sided organs). The uterus and both ovaries looked normal, no attachment with the cyst was identified. Gallbladder was retracted upward and the large cystic lesion was entirely visualized. It appeared to be an oval, thin walled and transparent. It had a regular border with smooth glistening surface containing about 500 ml of serous material. Cyst was easily separable from the adjacent organs. It was totally dissected from the inferior border of the liver and right kidney down to the right iliac fossa. Complete excision of the cyst was done followed by cholecystectomy. The cyst wall components and gallbladder were retrieved through the umbilicus (Figure 3). All her symptoms were disappeared after surgery.
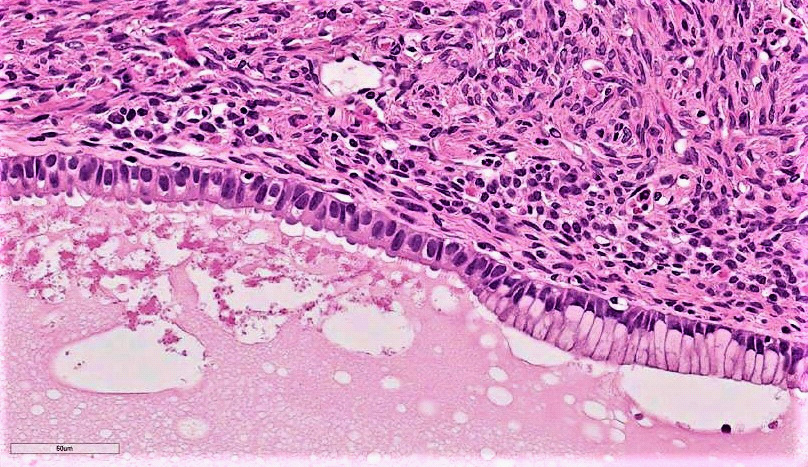
Histopathologic section revealed a thin walled multilocular cyst lined by tall columner cells with clear cytoplasm and basal nuclei along with low cuboidal cells resembling mesothelial cells. The stroma is densely cellular and collagenous, composed mainly of spindle cells. Microscopic examination was suggestive of mucinous cystadenoma with ovarian like stroma (Figure 4) No atypia or architectural complexity or any invasion was detected. Patient had an uneventful fast track recovery and 4 years' follow-up revealed no evidence of recurrence.
Discussion
Primary RCLs are unusual entity due to absence of epithelial cells in this region. They are heterogeneous and predominantly divided into solid and cystic lesions. They can be neoplastic lesions like cystic lymphangioma, mucinous cystadenoma, cystic teratoma, cystic mesothelioma, Mullerian cyst, epidermoid cyst, tailgut cyst and pseudomyxoma retroperitonei. It includes also nonneoplastic lesions like pancreatic pseudocyst, nonpancreatic pseudocyst, lymphocele, urinoma, and hematoma [1].
The widespread use of computed tomography (CT) for evaluating abdominal and retroperitoneal diseases has led to the increased detection rate for incidental RCL; however, the precise incidence of these lesions is still difficult to define. Nonneoplastic lesions are usually more frequent than neoplastic ones. RCLs are highly challenging regarding clinical presentation, diagnostics and the choice of therapeutic approaches. They manifest differently depending on their size and location. Abdominal pain, fullness or a palpable mass are the most common presenting complaint. Constitutional symptoms such as fever, changes in appetite, and weight loss may be present especially in malignant lesions [3]. Our patient denied any history of trauma or gynecologic issues, she was only complaining of abdominal discomfort leading to the further work-up and diagnosis.
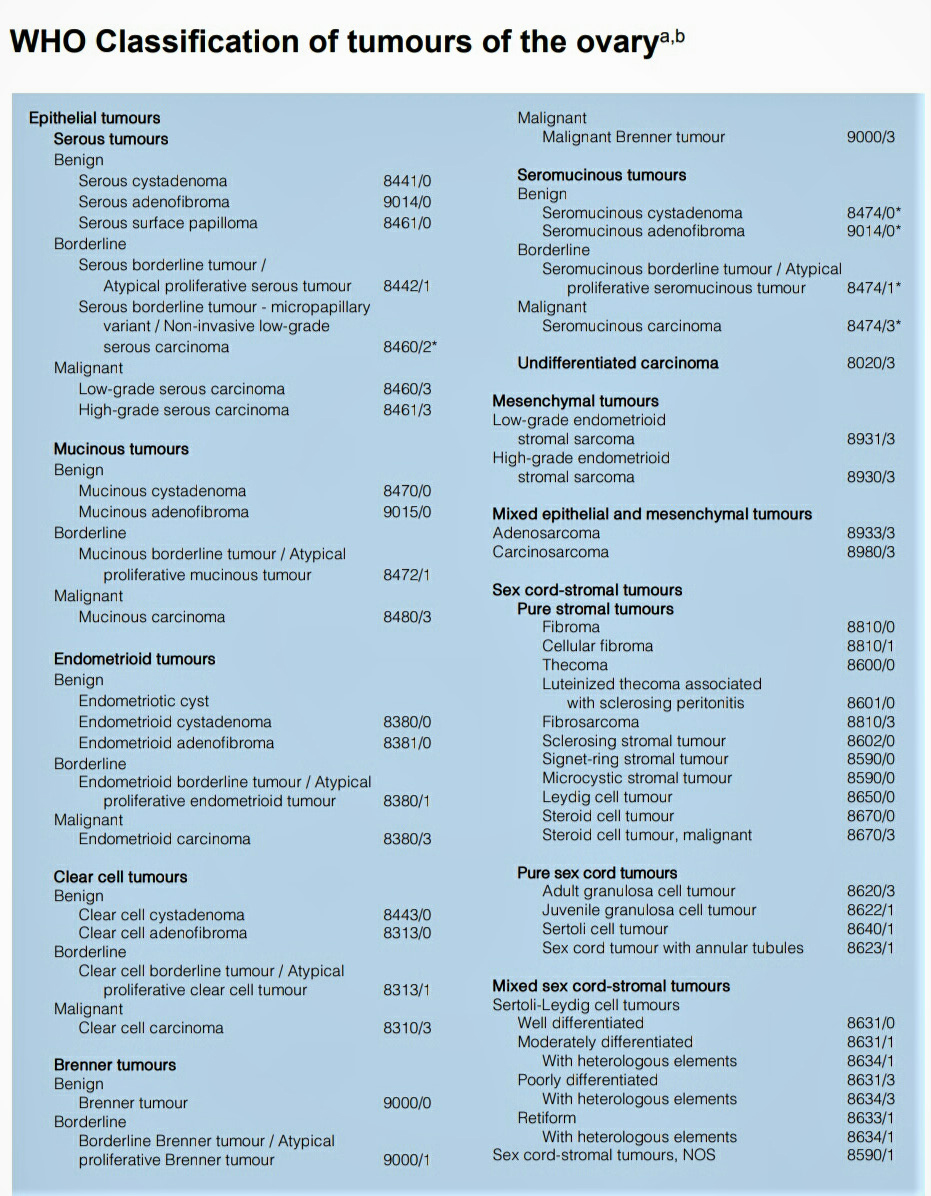
These masses arise within the retroperitoneal space, which is a complex region located behind the peritoneum [1,4]. This region houses few organs (such as the adrenal glands and kidneys, portions of the duodenum, pancreas and colon, and the esophagus), major vessels (the aorta and inferior cava vein), deep lymphatic vessels and structures, ligaments and fatty tissues [5]. RCLs remain a dilemma to clinicians as no clear diagnostic flow charts have been proposed thus far. That is why we decided to go for surgical option rather than observation and follow-up. Our case was successfully managed laparoscopicallyby complete excision of the cyst and histopathological examination was in favor of a primary retroperitoneal mucinous cystadenoma. These lesions had been named for a long time as Mullerian mixed cell tumor. Recently, the term mucinous neoplasm was introduced as a separate entity in the WHO 2014 (Figure 5) [6].
Primary Retroperitoneal Mucinous Cysts (PRMCs) are rare tumors with unclear origin. They share same morphologic features with ovarian mucinous cystadenomas except for presence of cuboidal cells that is a mesothelial marker supports its origin. They can also arise anywhere in the retroperitoneum but are unattached to the ovary [7]. PRMCs have the same macroscopic appearance of serous cystadenomas is usually composed of unilocular or multilocular cysts filled with clear or turbid watery fluid. The cysts measure 10 cm in average diameter, but may be extremely large [8]. In our case, the cyst was clear fluid filled unilocular with fine calcifications and absence of worrisome radiologic findings.
This histogenesis remains incompletely understood. However, two main assumptions have been postulated. According to the first, as there is similarity with ovarian mucinous cystadenoma, it is possible originated from an ectopic ovarian tissue however, ovarian like stroma was found in the cyst wall only in few cases [9] and have been also described in men as well [10]. The second hypothesis suggests that they originate from an invagination of multipotent mesothelial cells with subsequent mucinous metaplasia of the mesothelial cells [11]. Our case supports more the first hypothesis by containing ovarian like stroma in the absence of any attachment to the right ovary.
PRMCs are classified three histological types: 1) Benign type is the simple mucinous cystadenoma (most common); 2) Borderline type (least common) has an adjacent proliferative columnar epithelium and low malignant potential or carcinoma in situ. 3) Malignant type is the cystadenocarcinoma, which tend to recur and create metastasis [11,12]. Our patient had no atypia or no architectural complexity and no invasion was identified, hence the diagnosis of benign type was established. Our case luckily belongs to the benign type and its treatment is usually simple resection
Majority of described cases were treated surgically however the first laparoscopic excision of PRMC was performed by Chen on 1998 [13] and despite the availability of modern advanced techniques and expertise in minimally invasive surgery, laparoscopic approach still not widely tailored. We looked into the literature using the terms primary, retroperitoneal, mucinous, cystadenoma and laparoscopy. Searching in the title, abstract or keywords, a comprehensive review was conducted through Medline, Scopus, PubMed and Google Scholar (January 1989– August 2021) databases.
Only 16 cases of Laparoscopic PRMC resections were reported mostly females (14 out of 16) with different age, variable size and presentation (Table 1). All of them had been managed successfully with uneventful outcome.
Table 1: Cases of PRMC managed Laparoscopically (1989-2021).
| Study Group | Age | Sex | Presentation | Size cm | Treatment |
|---|---|---|---|---|---|
| Our Study 2021 | 55 | F | Rt Abdominal pain Palpable mass | 13 X 9 | Laparoscopy |
| Danen [14] 2020 | 19 | F | Asymptomatic | 6 X 4 | Laparoscopy |
| Chaves [15] 2019 | 62 | F | Abdominal pain | 612 X 8.5 | Laparoscopy |
| Koyama [16] 2019 | 41 | F | Abdominal pain | 5 X 3 | Laparoscopy |
| Lung [17] 2019 | 22 | F | Epigastric pain Nausea, vomiting | 9.5 X 8.5 | Laparoscopy |
| Foula [18] 2019 | 29 | F | Asymptomatic | 15 X 11 | Laparoscopy |
| Liu [19] 2019 | 56 | M | Abdominal pain | 9 X 3 | Laparoscopy |
| Pesapane [20] 2018 | 52 | F | Abdominal pain Palpable mass | 14 X 12 | Laparoscopy |
| Dayan [21] 2016 | 37 | F | Asymptomatic | 15 X 12 | Laparoscopy |
| Lee 1 [22] 2016 | 31 | F | Lt abdominal pain Palpable mass | 10 X 10 | Laparoscopy |
| Lee 2 [23] 2015 | 31 | F | LLQ pain | 6.5 | Laparoscopy |
| Paraskevakou 2014 [7] | 23 | F | Palpable mass | 9 X 6 | Laparoscopy |
| Mattei [24] 2013 | 32 | M | Palpable mass | 10 | Laparoscopy |
| Fujita [25] 2012 | 29 | F | Abdominal pain | 18 X 13 | Laparoscopy |
| Abedalthagafi 2009 [26] | 44 | F | Palpable mass | 11 X 7 | Laparoscopy |
| Arribas [27] 2004 | 39 | F | Asymptomatic | 10 X 9 | Laparoscopy |
| Chen [13] 1998 | 48 | F | Palpable mass | 15 X 13 | Laparoscopy |
Conclusion
RCLs are uncommon tumors with a large differential diagnosis. They usually remain silent until they grow into larger size. PRMC is a rare pathology in that region that constitutes a risk of infection and degeneration. Laparoscopy is becoming more widely accepted as a useful and safe treatment modality in this setting with careful preoperative evaluation to exclude malignancy.
Conflicts of interest: All authors declare no conflict of interest.
Funding: We report no involvement of sponsors.
Acknowledgements: Special thanks to our head of department Dr. Waleed Bouhaimed and our head of unit Dr Ali Taqi for their continuous support.
Consent: Written informed consent was obtained from the patient and is available upon request.
References
- Yang DM, Jung DH, Kim H, et al: Retroperitoneal cystic masses: CT, clinical and pathologic findings and literature review. Radiographics. 2004; 24: 1353-65.
- Savitri Nerune RM. Potekar, Varsha R. Deshpande, et al: Seromucinous cystadenoma of ovary: A rare case report. JKIMSU, Juoly-September 2017; 6: 3.
- Amit Mori, Kinesh Changela, Dhuha Alhankawi et al: A Giant Primary Retroperitoneal Serous Cystadenoma: Case Report and Review of Retroperitoneal Cysts. Surg J. 2017; 3: e32–e37.
- Osman S, Lehnert BE, Elojeimy S et al: Comprehensive review of the retroperitoneal anatomy, neoplasms and pattern of disease spread. Curr Probl Diagn Radiol. 2013; 42: 191–208.
- Tirkes T, Sandrasegaran K, Patel AA, et al. Peritoneal and retroperitoneal anatomy and its relevance for cross-sectional imaging. Radiographics. 2012; 32: 437–451.
- Kurman RJ, Carcangiu ML, Herrington CS, et al: WHO classification of Tumours of Female Reproductive Organs, WHO classification of Tumours. International agency for Research on Cancer [IARC], 4th edition, Volume 6.
- Paraskevakau H, Orfanos S, Diamantis T, et al: Primary retroperitoneal mucinous cystadenoma. A rare case with two cysts and review of the literature. Hippokratia. 2014; 18: 278-281.
- Navin P, Meshkat B, McHugh S, et al: Primary retroperitoneal mucinous cystadenoma - A case study and review of the literature. International Journal of Surgery Case Reports. 2012; 3; 486-488.
- Lai KKT, Chan YYR, Chin ACW, Ng WF, Huang YHH, Mak YLM, et al. Primary retroperitoneal mucinous cystadenoma in a 52-year-old man. Journal of Hong Kong College Of Radiologists. 2004; 7: 223-5.
- Tapper EB, Shrewsberry AB, Oprea G, Majmudar B. A unique benign mucinous cystadenoma of the retroperitoneum: A case report and review of the literature. Archives of Gynecology and Obstetrics. 2010; 281: 167-9.
- Min BW, Kim JM, Um JW, et al: The First Case of a Retroperitoneal Mucinous Cystadenoma in Korea: A Case Report. The Korean Journal of Internal Medicine. 2004; 19: 282-284.
- Matsubara M, Shiozawa T, Tachibana R, et al. Primary retroperitoneal mucinous cystadenoma of borderline malignancy: A case report and review of the literature. International Journal of Gynecological Pathology. 2005; 24: 218-23.
- Chen JS, Lee WJ, Chang YJ, Wu MZ, Chiu KM. Laparoscopic resection of a primary retroperitoneal mucinous cystadenoma: report of a case. Surg. Today. 1998; 28: 343–345.
- Danen C, Leschke T, Bassi D, Sharma R. First Report of Retroperitoneal Mucinous Cystadenoma in a Patient with Hirsutism. Clin Med Res. 2020; 18: 27-32.
- Chaves MM, Castro R, Mota-Vieira L, Carneiro V. A rare case of a primary retroperitoneal mucinous cystic tumour with borderline malignancy and literature review. BMJ Case Rep. 2019; 12: e230708.
- Koyama R, Maeda Y, Minagawa N, Shinohara T, Hamada T. Laparoscopic Resection of a Primary Retroperitoneal Mucinous Cystadenoma. Case Rep Gastroenterol. 2019; 13: 159-164.
- Lung J, Gracey A, Rosales A, et al. Laparoscopic excision of a retroperitoneal mucinous cystic neoplasm: A case report. Int J Surg Case Rep. 2019; 62: 27-30.
- Foula MS, AlQattan AS, AlQurashi AM, AlShaqaq HM, Mirza Gari MK. Incidentally discovered huge retroperitoneal mucinous cystadenoma with successful laparoscopic management: Case report. Int J Surg Case Rep. 2019; 61: 242-245.
- Liu K, Chang Y, Lin Y, Kao C, Chang J. Primary Retroperitoneal Mucinous Cystadenoma with Borderline Malignancy Concerning in Male Patient: A Case Report and Literature Review. 2019.
- Pesapane F, Van Renterghem S, Patella F, De Visschere P, Villeirs G. A case report and a literature review of primary retroperitoneal mucinous cystadenoma: the importance of imaging in diagnosis and management. Future Oncol. 2018; 14: 2923-2931.
- Dayan D, Abu-Abeid S, Klausner JM, Sagie B. Primary Retroperitoneal Mucinous Cystic Neoplasm: Authors' Experience and Review of the Literature. Am J Clin Oncol. 2016; 39: 433–440.
- Lee SY, Han WC. Primary Retroperitoneal Mucinous Cystadenoma. Annals of Coloproctology. 2016; 32: 33-37.
- Lee SE, Oh HC, Park Y-G, Choi YS, Kim MK. Laparoscopic excision of primary retroperitoneal mucinous cystadenoma and malignant predicting factors derived from literature review. International Journal of Surgery Case Reports. 2015; 9: 130-133.
- Mattei J, Kim FJ, Phillips J Et al. Male primary retroperitoneal mucinous cystadenoma. Urology. 2013; 82: e1–e2.
- Fujita K, Yamamoto Y, Yamaguchi S. Laparoscopic resection of primary retroperitoneal mucinous cystadenoma by retroperitoneal approach. Int. J. Urol. 2011; 18: 607–608.
- Abedalthagafi M, Jackson PG, Ozdemirli M. Primary retroperitoneal mucinous cystadenoma. Saudi Med. J. 2009; 30: 146–149.
- Arribas D, Cay A, Latorre A, Cordoba E, Martinez F, Lagos J. Retroperitoneal mucinous cystadenoma. Arch Gynecol. Obstet. 2004; 270: 292–293.